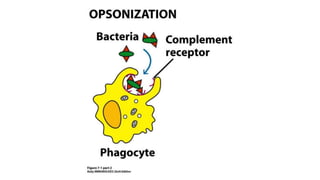
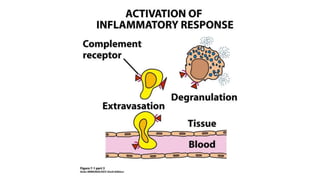
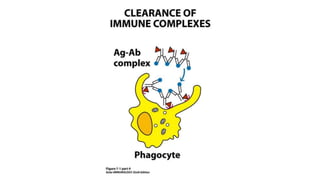
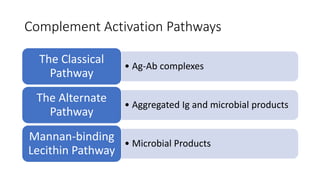
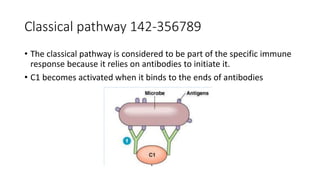
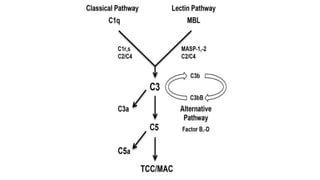
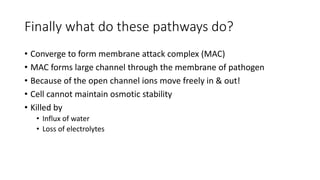
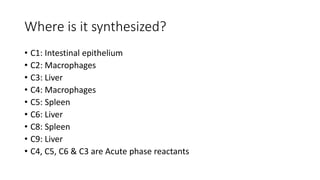
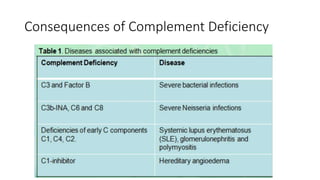
The complement system consists of over 30 proteins produced by the liver and found in circulating blood serum. It works as a cascade system where one reaction triggers another rapidly. The complement system plays a critical role in inflammation and defense against some bacterial infections, and may be activated during blood transfusions or autoimmune diseases. There are three complement activation pathways: the classical pathway which is initiated by antigen-antibody complexes, the alternative pathway which can be triggered by pathogens, and the lectin pathway which is initiated when mannose-binding lectin binds to carbohydrates on bacteria. All three pathways converge to form the membrane attack complex, which creates pores in the pathogen's membrane leading to cell death.