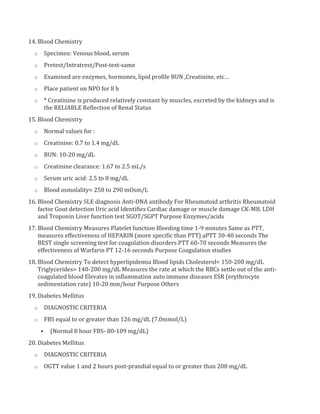
1. Common laboratory procedures include blood tests, urine and stool exams, imaging tests, and biopsies. Blood tests often involve blood draws to check electrolytes, blood counts, chemistries and more.
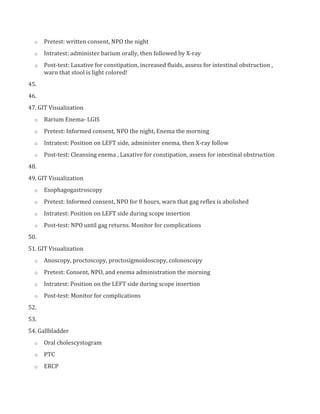
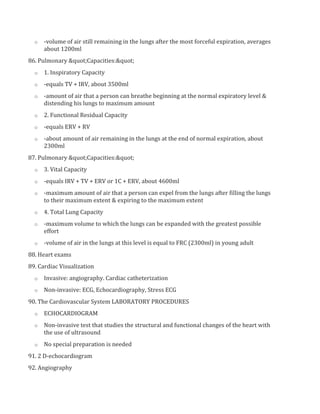
2. Imaging tests allow visualization of internal organs and structures and include procedures like X-rays, ultrasounds, CTs and MRIs. More invasive visualization tests include procedures like bronchoscopy, cystoscopy and angiography.
3. Biopsy and aspiration procedures remove fluid or tissue samples for examination and include lumbar puncture, abdominal paracentesis and bone marrow aspiration. These invasive procedures require informed consent.