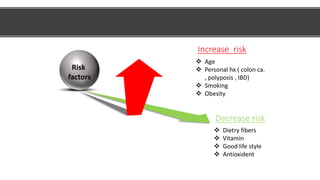
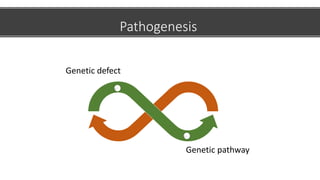
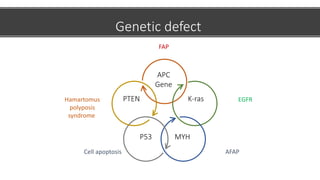
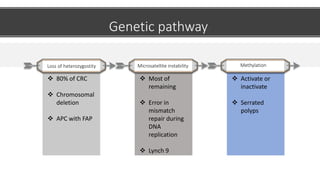
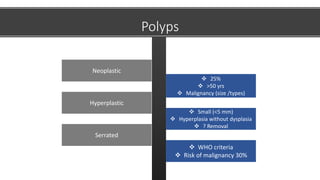
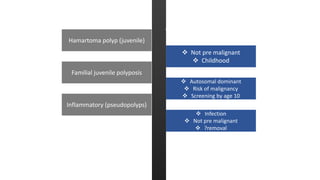
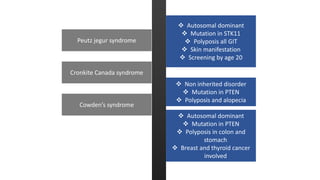
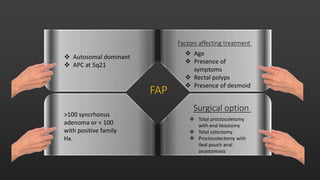
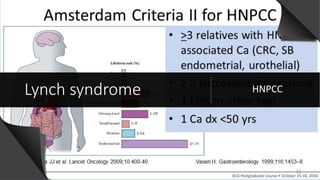
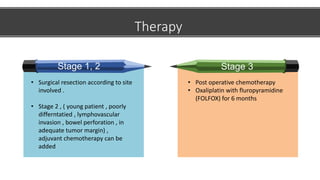
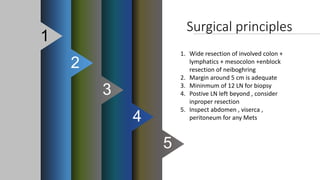
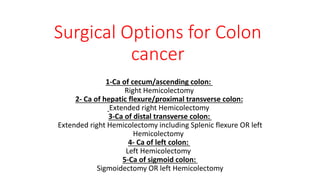
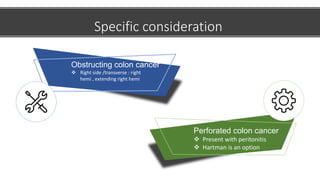
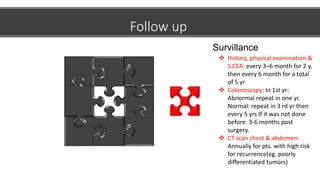
This document discusses colon cancer, including risk factors, pathogenesis, types of polyps, staging, and treatment. The main risk factors for colon cancer are age, personal history of colon cancer or inflammatory bowel disease, smoking, and obesity. Genetic defects like in the APC gene can cause familial adenomatous polyposis (FAP). Colon cancer is typically staged after diagnosis and treatment may involve surgery like colectomy along with chemotherapy and follow-up surveillance colonoscopies.