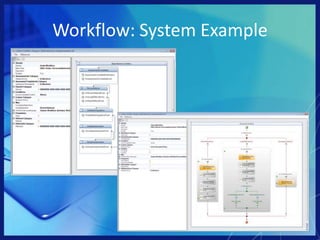
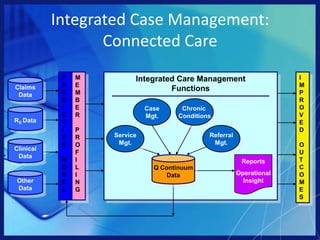
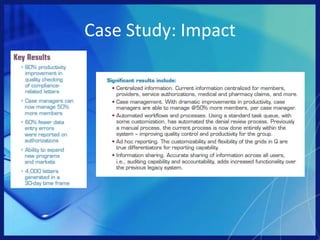
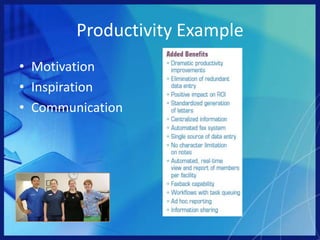
This document discusses how technology can help streamline case manager processes and improve outcomes. It evaluates the current healthcare environment and how technology advances like workflows and dashboards can enhance productivity. It also presents a case study where collaboration technology helped a managed care provider eliminate paper-based systems and improve productivity and customer service. The document advocates that organizations evaluate how technology can improve quality of care.