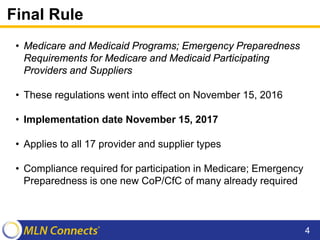
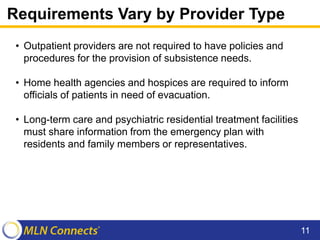
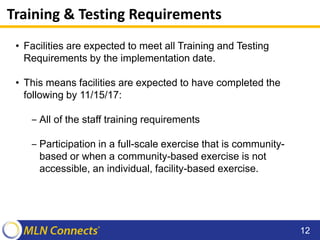
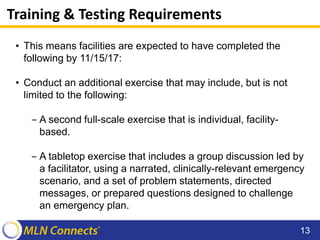
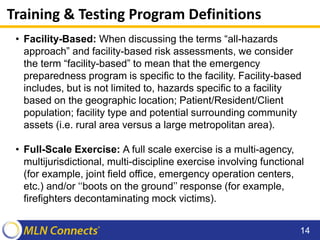
This document summarizes the requirements of the Emergency Preparedness Final Rule for Medicare and Medicaid participating providers and suppliers. It discusses the four key provisions that all provider types must have: risk assessment and planning, policies and procedures, communication plans, and training and testing. It provides definitions of terms and outlines that all facilities must be compliant with training and testing exercises, including an initial full-scale community exercise, by November 15, 2017. Questions from participants are then answered.