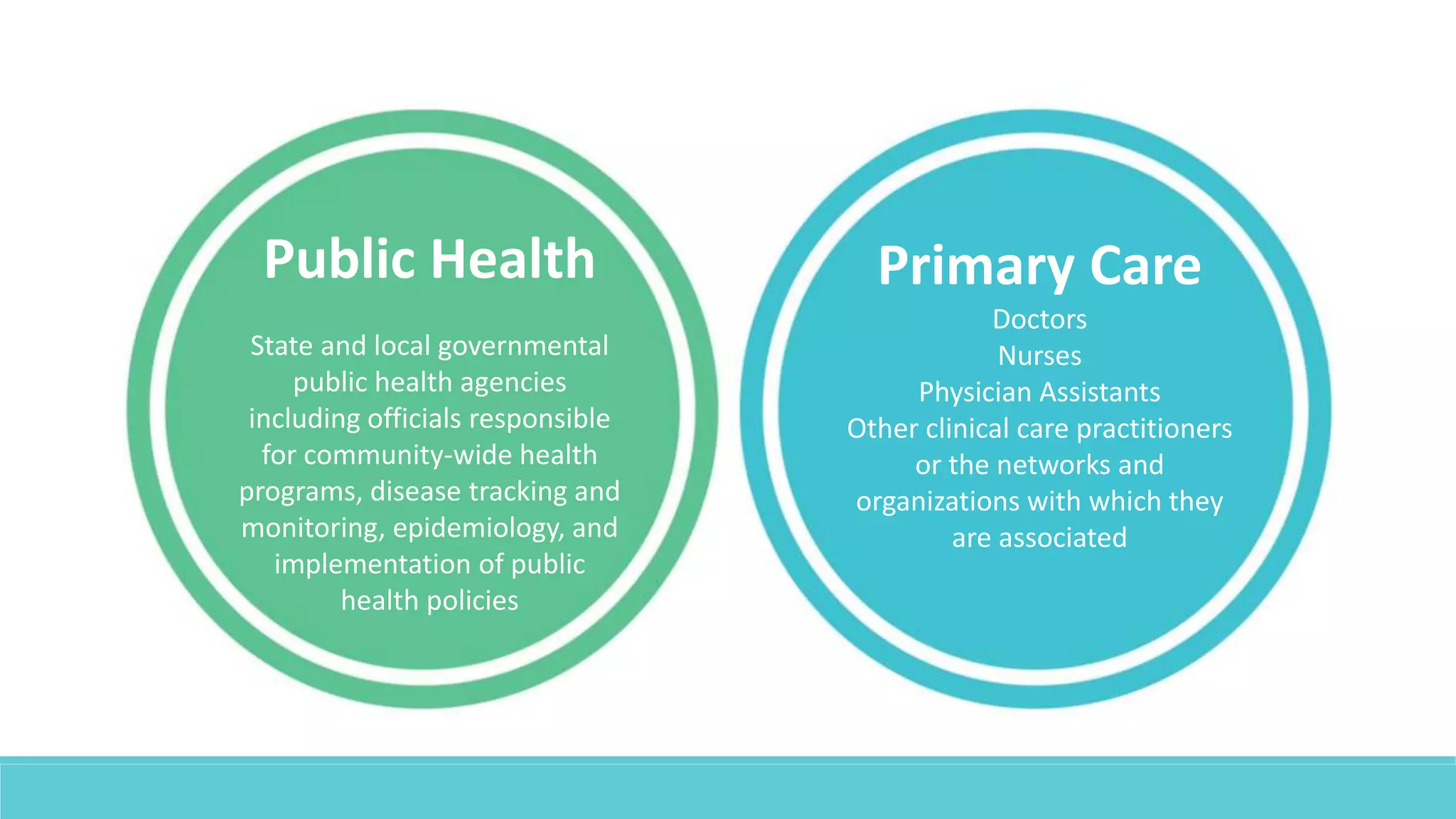
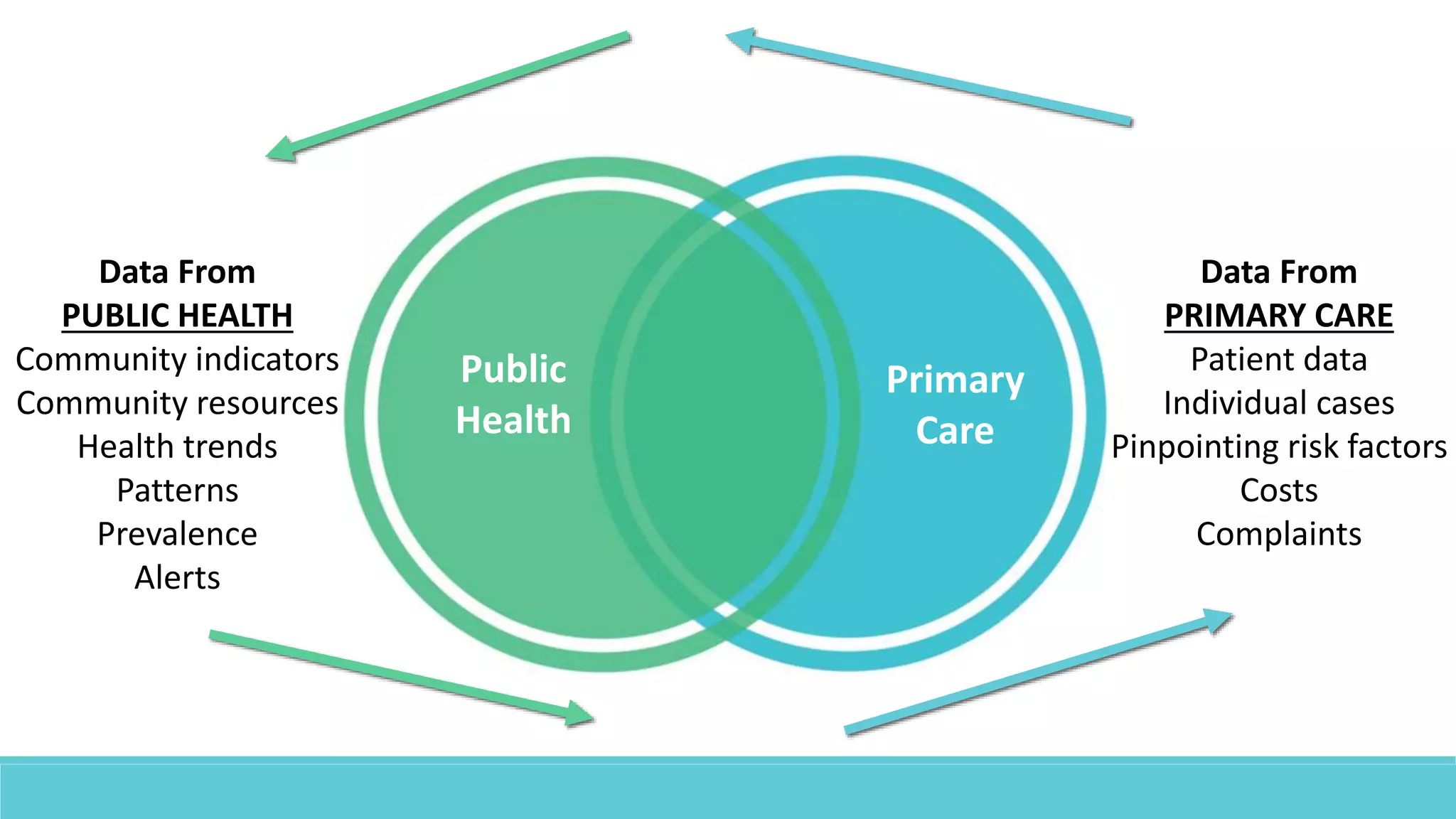
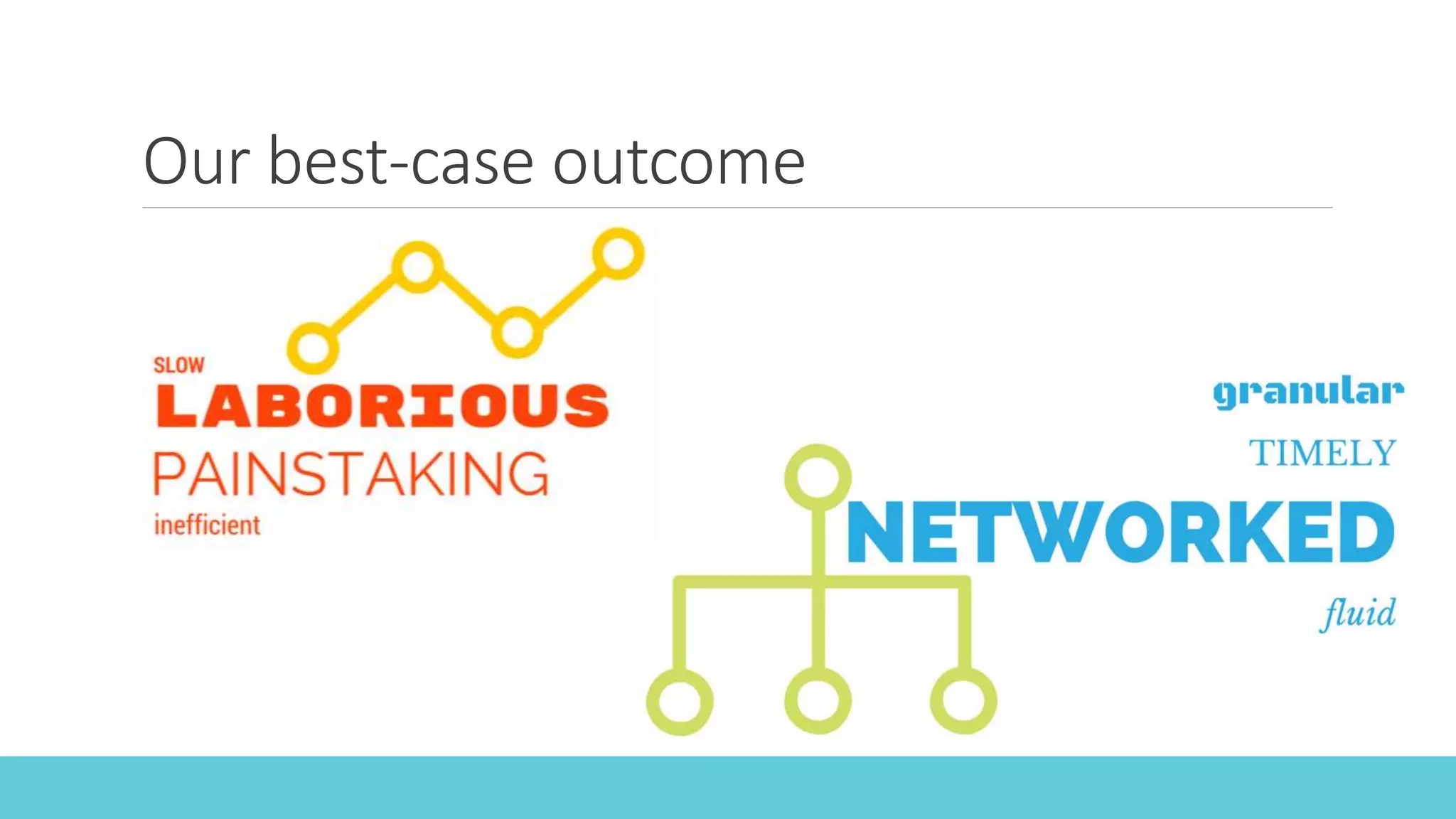
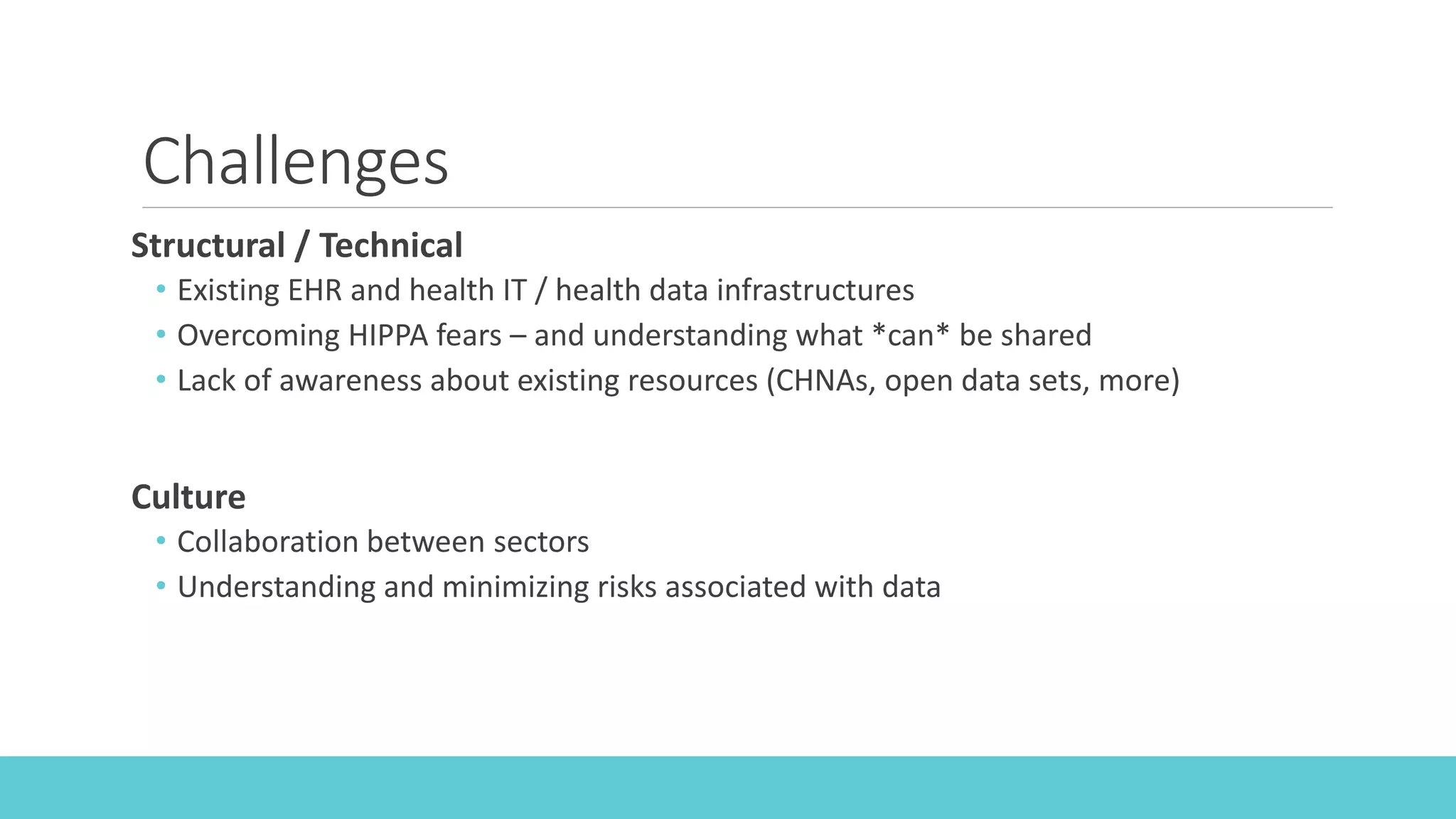
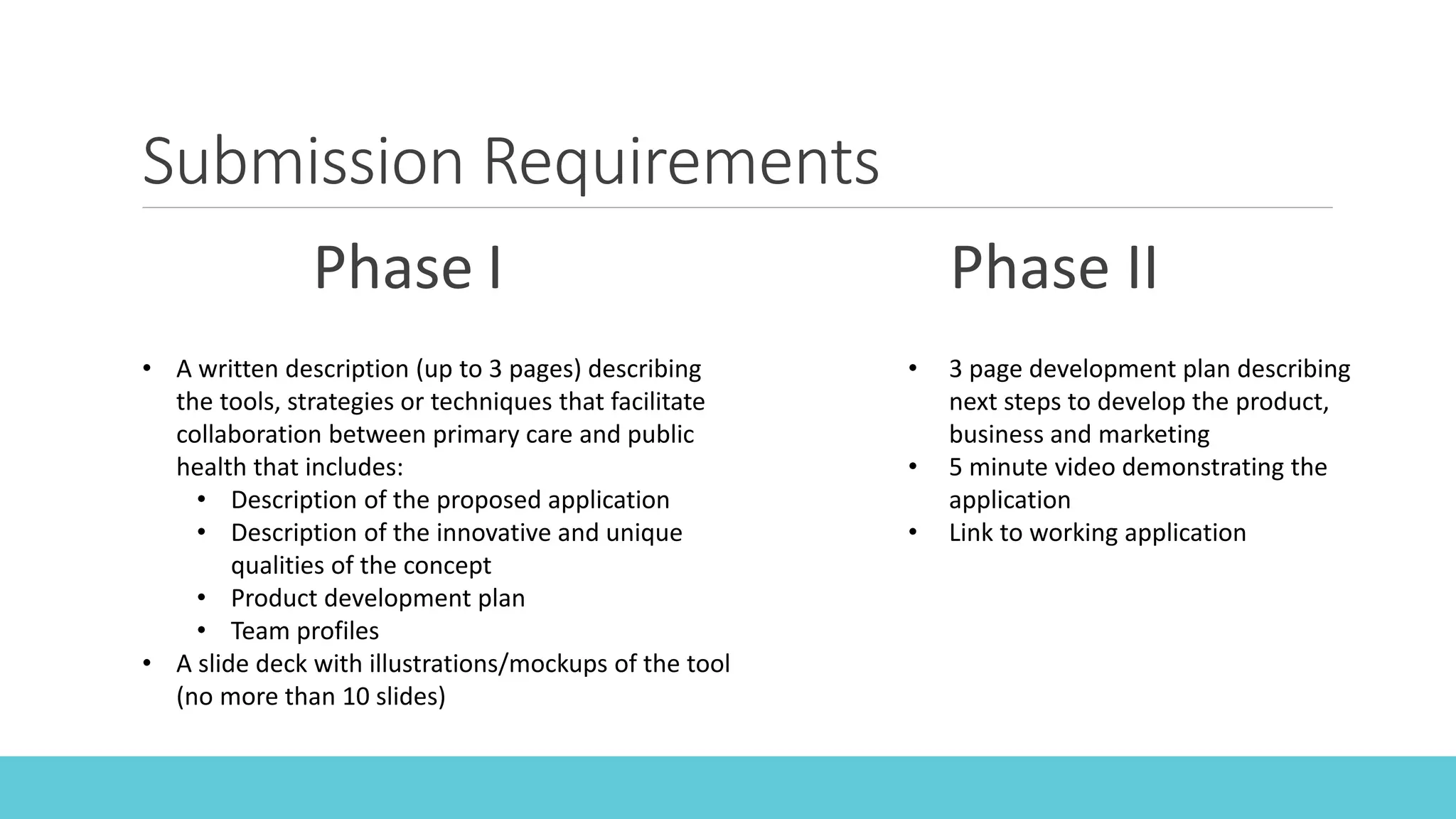
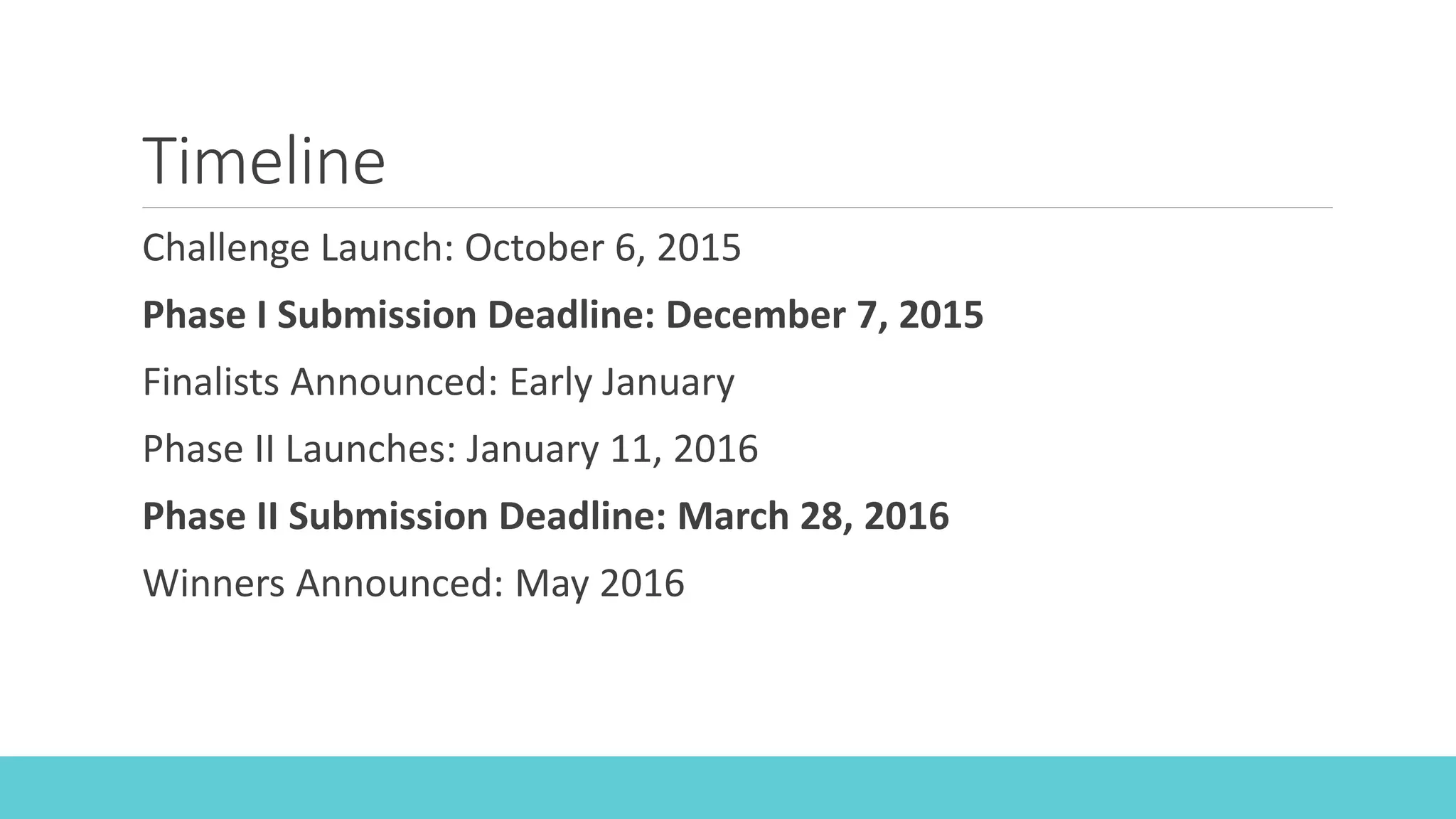
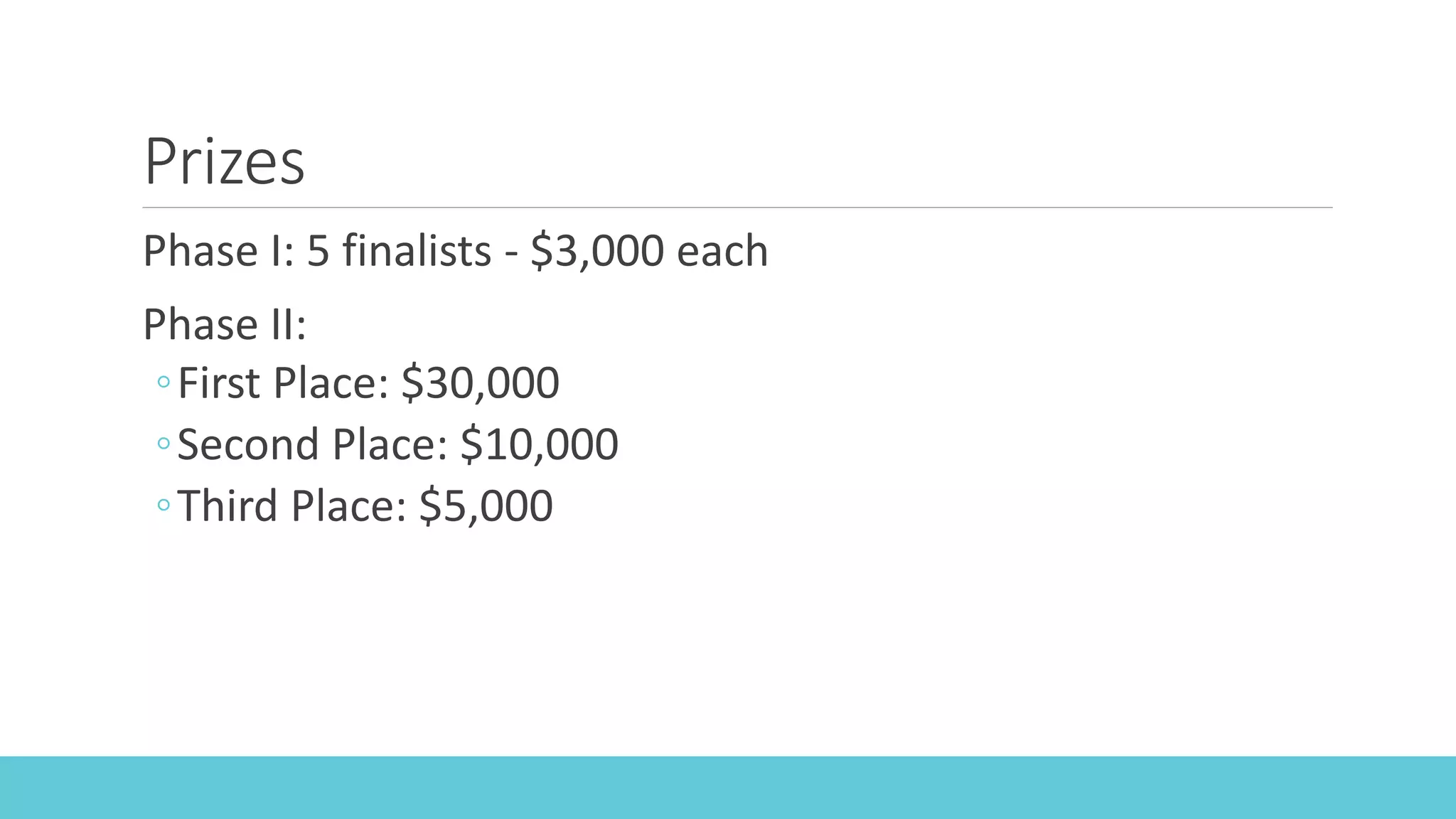
This webinar introduces the Closing the Data Divide Challenge to develop tools that facilitate data sharing between primary care and public health. The challenge is sponsored by the de Beaumont Foundation and Health 2.0. Participants are asked to submit proposals in two phases - with the first phase focusing on describing a proposed tool and the second developing a working application. Finalists in Phase I will receive $3,000 and winners in Phase II will receive prizes from $5,000 to $30,000. The goal is to create sustainable connections between primary care and public health to improve population health by leveraging their respective data and skills. Challenges to data sharing include technical infrastructure limitations and cultural barriers to collaboration that solutions should seek