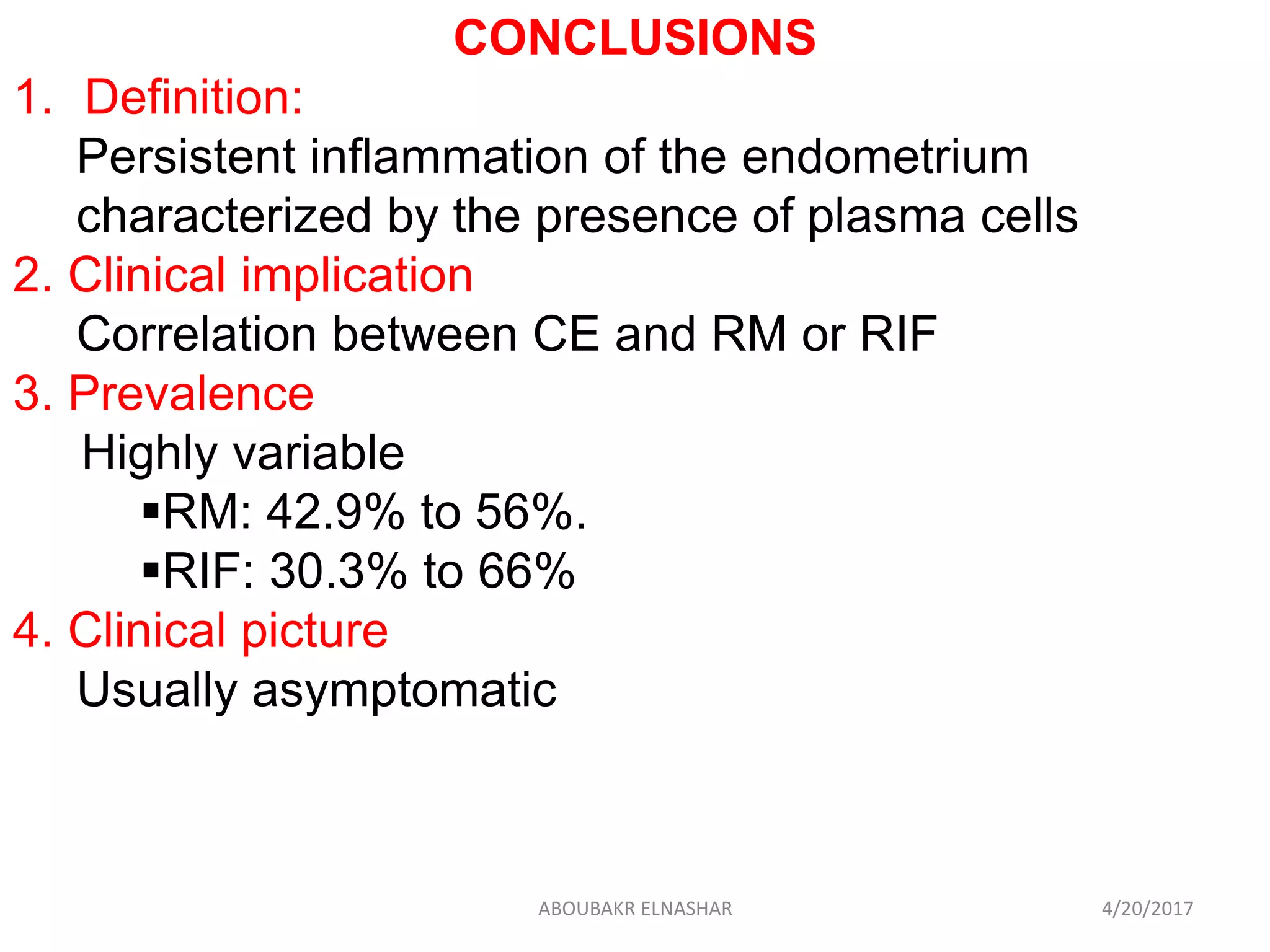
Chronic endometritis (CE) is a persistent inflammation of the endometrial lining characterized by the presence of plasma cells. CE has been correlated with repeated miscarriage (RM) and repeated implantation failure (RIF), with prevalence rates ranging from 42.9-56% in RM and 30.3-66% in RIF. CE is typically diagnosed through histological examination of an endometrial biopsy sample using hematoxylin and eosin staining or immunohistochemistry, though office hysteroscopy may also be used. Treatment with a 2 week course of antibiotics such as ofloxacin or doxycycline results in histological cure in 70-95% of cases and significantly improves live birth rates in
![Mechanism
Altered endometrial receptivity by
1. Abnormal infiltration of plasma cells
2. Secretion of IgM, IgG, and IgA antibodies
(Kasius et al, 2011).
3. Alteration in:
Endometrial cytokine production
[Maybin et al, 2011],
Secretion of paracrine factors
[Matteo et al, 2009, Di Pietro et al, 2013].
Endometrial expression of genes
(Johnston-MacAnanny, 2010).
4. Delay differentiation of the EM in the mid-
secretory phase (out-of-phase morphology)
[Mishra et al, 2008].
4/20/2017ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/chendometritis-170420060947/75/Chronic-Endometritis-in-Repeated-miscarriage-and-Repeated-implantation-failure-10-2048.jpg)
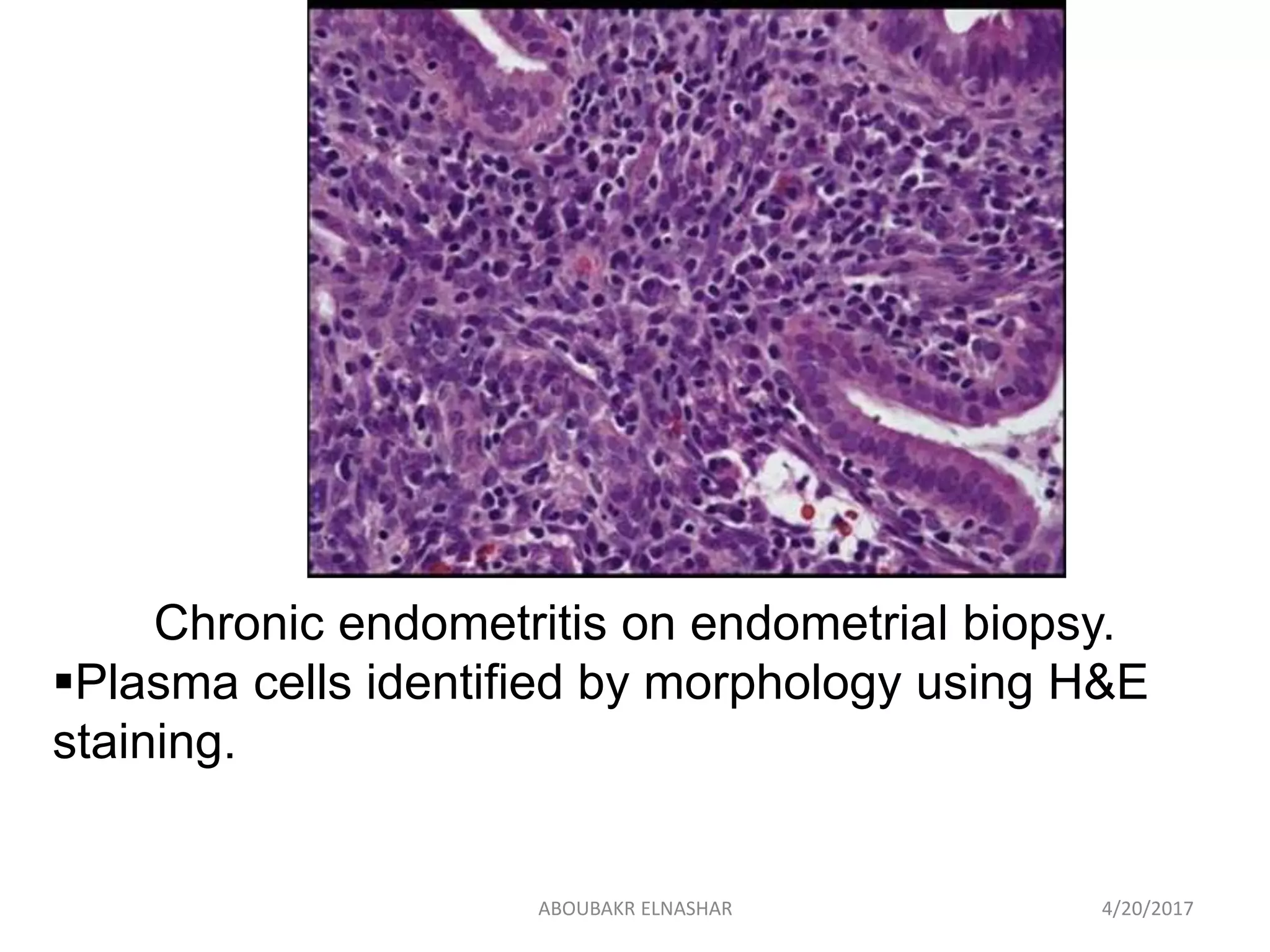
![1. Histologic diagnosis using H&E
Gold standard for the diagnosis
(Kasius et al.,2011)
Time-consuming and difficult.
Low diagnostic rate (<10%)
[Kasius et al, 2011, McQueen et al, 2014]
±miss the diagnosis.
{normal presence of leukocytes in the
endometrium especially before
menstruation}
[Kasius et al, 2012].
± over diagnosis
{Plasma cells can appear morphologically
similar to other stromal cells and leukocytes}
(Greenwood, Moran, 1981).
4/20/2017ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/chendometritis-170420060947/75/Chronic-Endometritis-in-Repeated-miscarriage-and-Repeated-implantation-failure-15-2048.jpg)
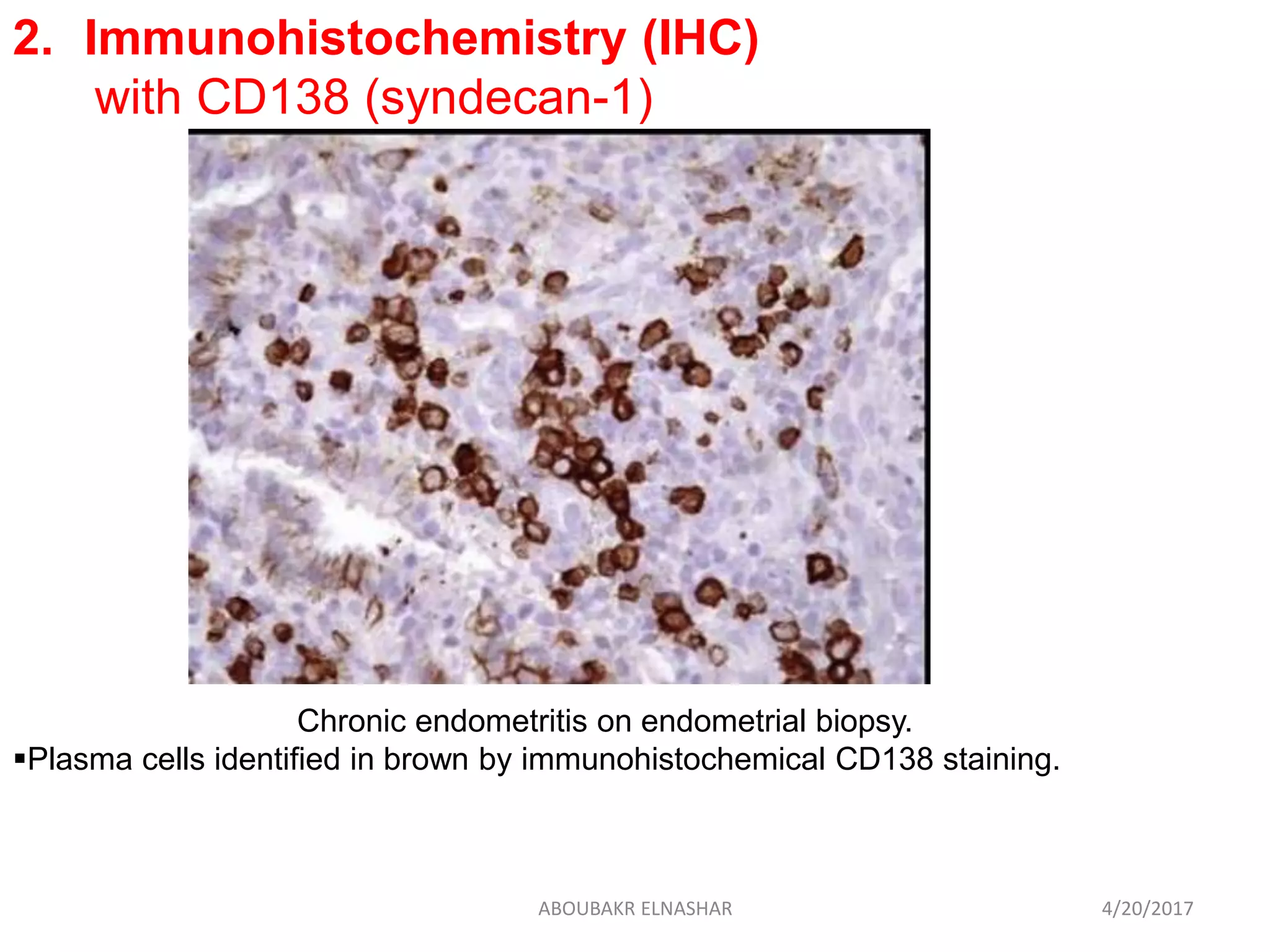
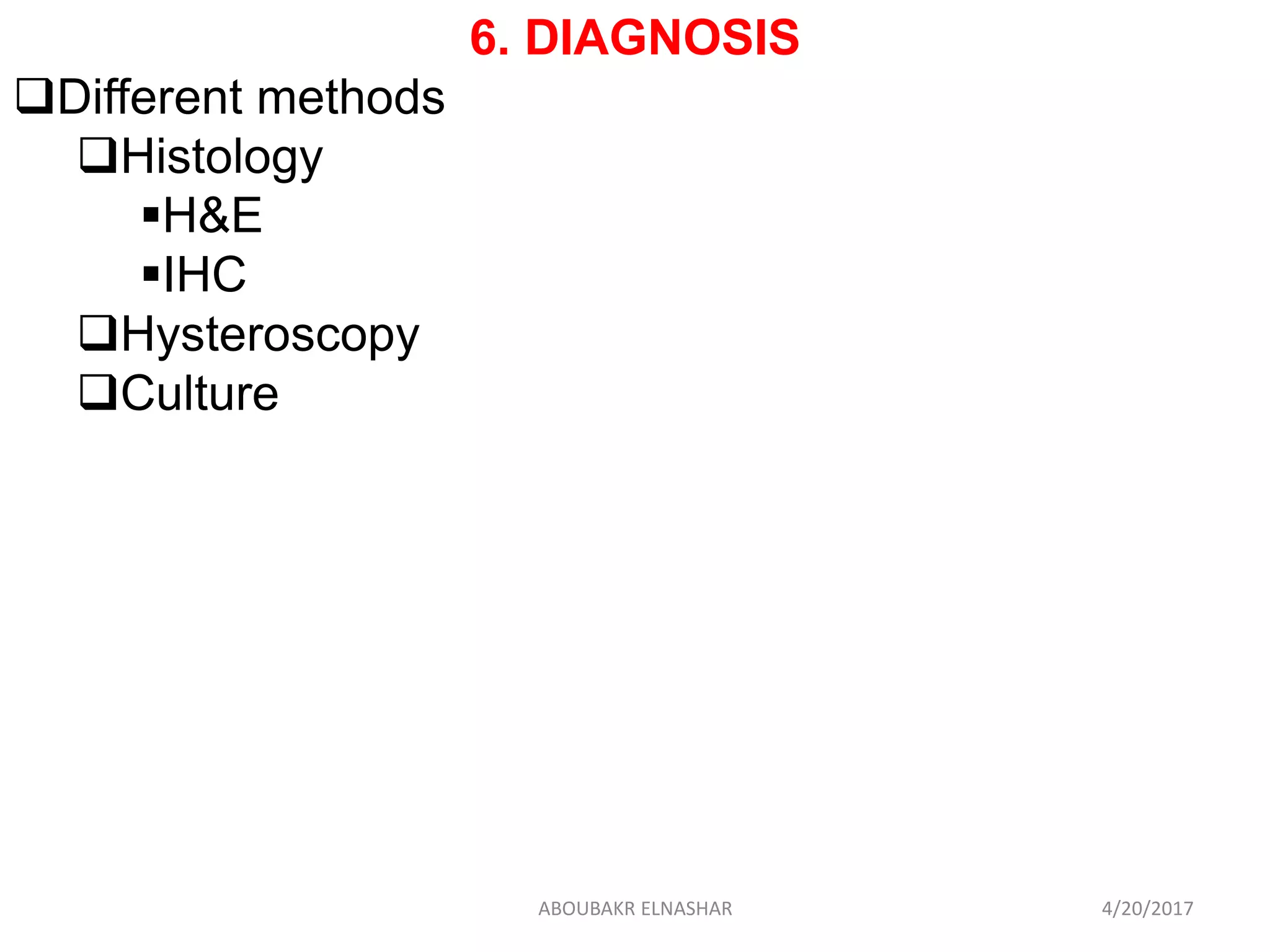
![Higher sensitivity
56%, as compared to a 13%for H&E staining
[McQueen et al, 2015].
(Miguel et al, 2011)
More accurate:
(Bayer-Garner et al, 2001).
Reducing false-negative diagnosis
(McQueen et al.2014)
Not yet recommended in daily clinical practice
Not widely used for the diagnosis of CE
IHCH&E
100%75%Sensitivity
100%65%Specificity
4/20/2017ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/chendometritis-170420060947/75/Chronic-Endometritis-in-Repeated-miscarriage-and-Repeated-implantation-failure-19-2048.jpg)
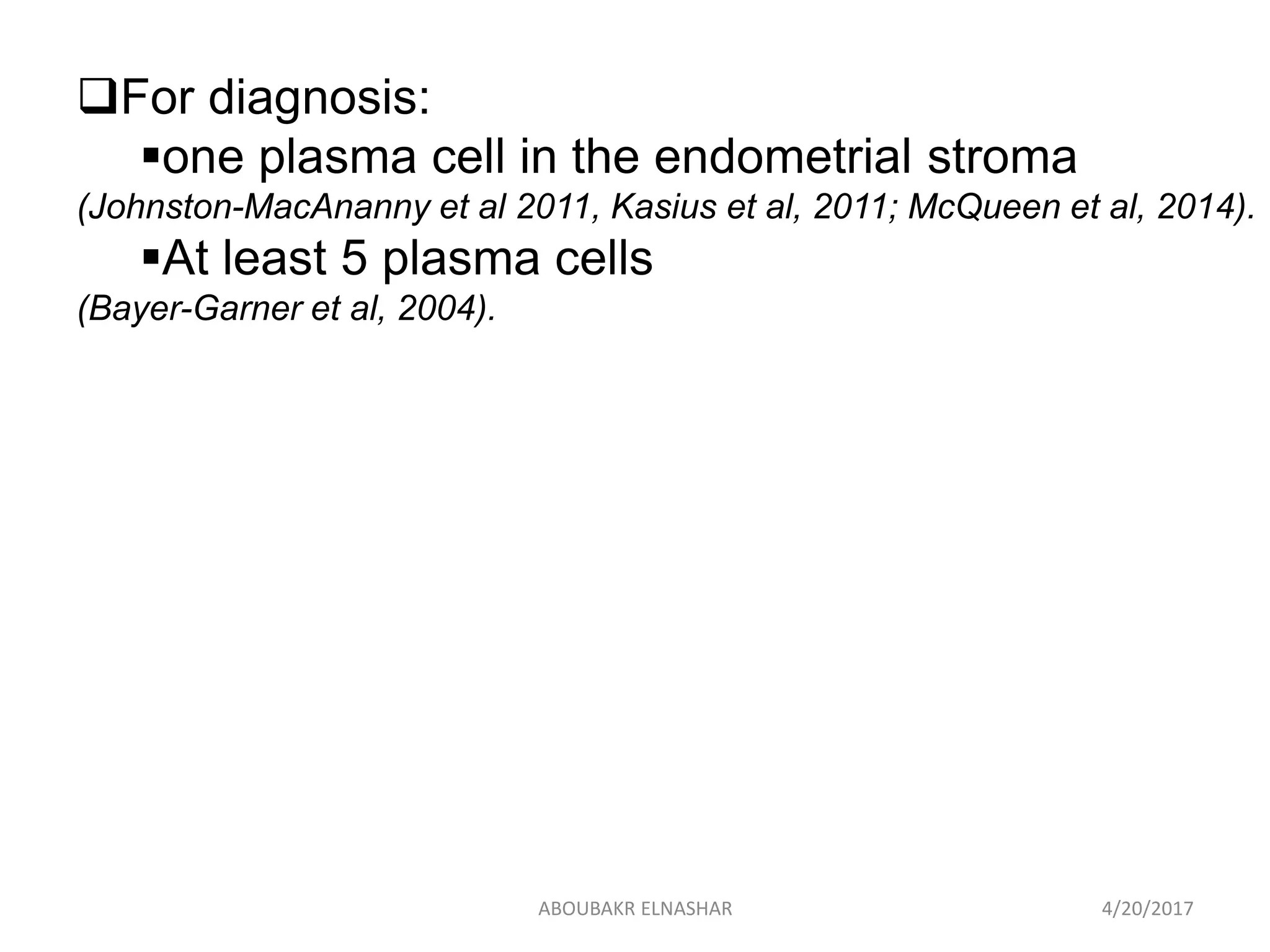
![Sensitivity:
40%
(Bouet et al, 2016).
much greater sens
Specificity
80%
(Bakas et al, 2014; Bouet et al, 2016)
dependent on the clinician's experience
Accuracy
93.4%
[Cicinelli et al, 2008,2010].
Normal hysteroscopy
relatively accurate predictor of successful pregnancy
after ART
[Cicinelli et al , 2015].
4/20/2017ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/chendometritis-170420060947/75/Chronic-Endometritis-in-Repeated-miscarriage-and-Repeated-implantation-failure-23-2048.jpg)
![4. Culture:
Positive in 75% of histologically confirmed CE
Common bacteria:
Escherichia coli, Enterococcus faecalis
Streptococcus agalactiae: 77.5%
Mycoplasmae/Ureaplasma: 25%
Chlamydia: 13%
(Cicinelli et al, 2014).
Often a causal organism cannot be identified.
CE have no correlation with
Bacterial colonization of the EM or
Clinical presentation of PID
[Korrn et al, 1995; Andrews et al, 2005].
4/20/2017ABOUBAKR ELNASHAR](https://image.slidesharecdn.com/chendometritis-170420060947/75/Chronic-Endometritis-in-Repeated-miscarriage-and-Repeated-implantation-failure-24-2048.jpg)