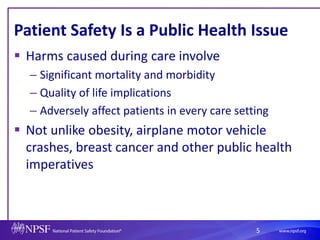
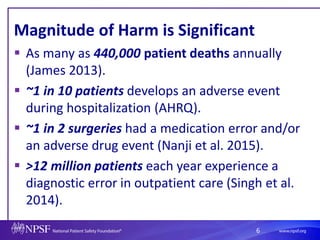
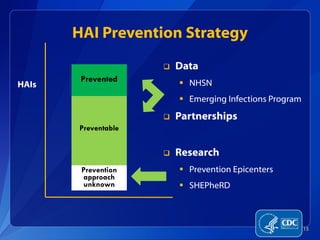
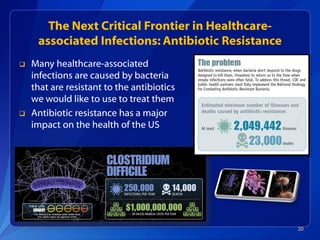
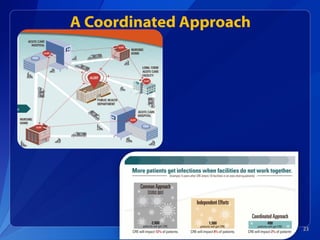
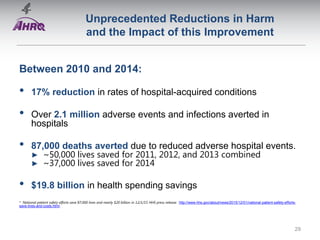
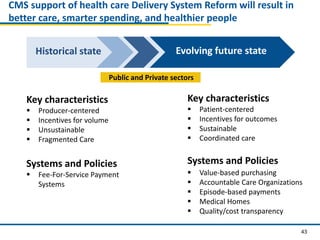
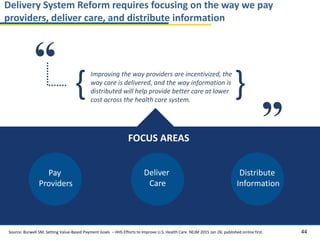
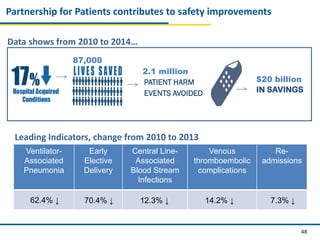
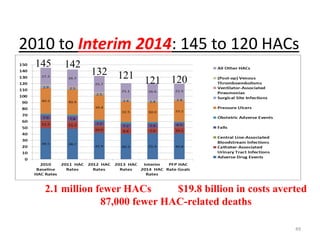
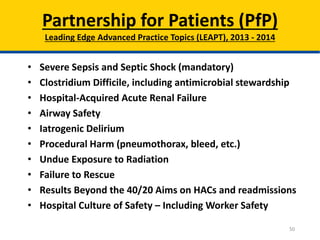
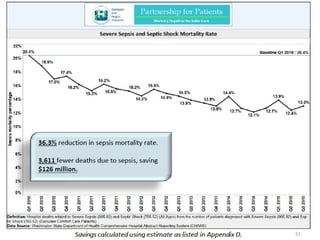
Patient Safety Awareness Week highlights the crucial role of all healthcare professionals in ensuring patient safety, addressing significant public health issues such as healthcare-associated infections and medical errors. Statistics reveal alarming rates of patient harm, with thousands of deaths and adverse events occurring annually, stressing the necessity for collaborative efforts in safety improvement. Ongoing initiatives like the Partnership for Patients have shown promising results in reducing hospital-acquired conditions and promoting a culture of safety within the healthcare system.