The document introduces psychopharmacology, emphasizing its complexity and the necessity for mental health professionals to integrate knowledge of brain science, pharmacodynamics, and cultural factors in understanding psychotropic medications. It encourages readers to embrace the complexities of the mind and brain while learning about the advances in neuroscience that have influenced drug development. The authors advocate for a comprehensive approach to psychopharmacology that goes beyond mere medical models, incorporating diverse perspectives to enhance clinical practice.






























































![many of these drugs is modest at best. [For example, meta-
analyses suggest antidepressants are only better than placebo
50% of the time (Khan, Leventahl, Khan, & Brown, 2002).]
Another problem has been a steep increase in the number of
lawsuits and amounts in settlements where companies were
fined for questionable practices linked to psychotropic
medications. In 2012 alone, companies paid over $5 billion in
fines related to allegations of fraud including misleading claims
about drug safety (Associated Press, 2009; Isaacs, 2013). That
said, it remains to be seen how much new research will be done
on pharmacological interventions because we know that mental
and emotional disorders are more complex than brain chemistry.
Certainly current medications that target receptors sites will be
used for symptom control so understanding binding is still
important. Until we can understand the etiology of mental
disorders, symptom control may be the best we can do.
Although we know from Chapter Two that drugs bind to
receptors to cause main effects, it is important to note that
drugs may also bind at sites where there appear to be no
measurable effects. These sites are called drug depots and they
include plasma protein, fat and muscle. Depot binding does
effect drug action in that it decreases the concentration of the
drug at sites of action because only freely circulating drugs can
pass across membranes. Also because these molecules will
eventually unbind and re-enter bloodstream it can lead to
higherthan-expected plasma levels and in some cases drug
overdose (Meyer & Quenzer, 2005).
Types of Tolerance
It is important to generally understand the types of tolerance
clients can develop to drugs. Please note that in this book we
avoid using the word “addiction.” The emotional hysteria
around this word, and the lack of operational definitions, make
it too inexact to be helpful. Physical dependence is linked with
the term addiction and implies that withdrawal signs are “bad”
and only linked to drugs of abuse. This is far from the truth
because severe withdrawal signs can follow cessation of such](https://image.slidesharecdn.com/chapteroneintroductionlearningobjectivesbeabletoconcept-221119173534-5fdf2160/85/CHAPTER-ONEIntroductionLearning-Objectives-Be-able-to-concept-docx-82-320.jpg)




![ITIS
Presentation Hints
Use dot points
Forces you not to read the slide, but to paraphrase
Describe using diagrams if that is easier
Raise and Lower the pitch of your voice
Make it more interesting to listen to
Time it correctly (ie practice it)
With Powerpoint, you can replace the voice on each slide
separately, if you mess up
Suggestion to vastly reduce MP4 file size
Use ffmpeg as follows
> ffmpeg -i %infile% -c:v libx264 -crf 50 -b 24k -ac
%outfile%.mp4
RMIT University, COSC2737 IT Infrastructure & Security
Assignment 1: Presentation Overview
11
ITIS
Interplanetary File System
Jill A Student, [email protected]
Presented as part of Assignment 1 for
COSC2737 IT Infrastructure and Security
Semester 1, 2020](https://image.slidesharecdn.com/chapteroneintroductionlearningobjectivesbeabletoconcept-221119173534-5fdf2160/85/CHAPTER-ONEIntroductionLearning-Objectives-Be-able-to-concept-docx-94-320.jpg)
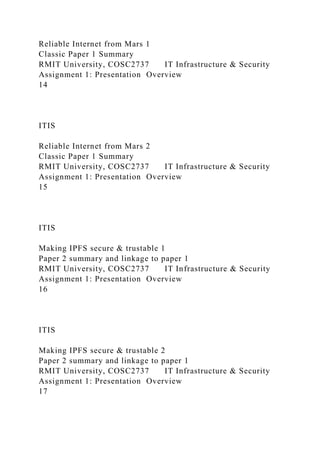

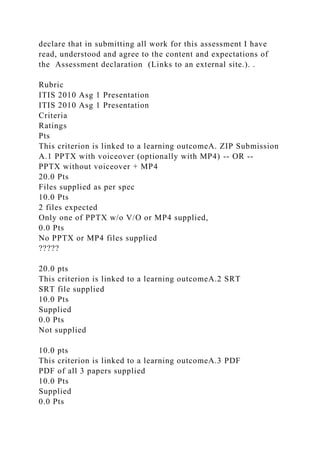



![Jill A Student, [email protected]
Presented as part of Assignment 1 for
COSC2737 IT Infrastructure and Security
Semester 1, 2020
ITIS
Overview
The problem of reliable insterplanetary communication where
transmission latency is significant
Classic Paper: Reliable Internet from Mars
The InterPlaNetary Internet: a communications infrastructure
for Mars exploration
Making IPFS secure and trustable
BlockIPFS-Blockchain-enabled Interplanetary File System for
Forensic and Trusted Data Traceability
…and you thought your IoT didn’t have the range !!
An InterPlanetary File System (IPFS) based IoT framework
Security Hacks
NASA’s Jet Propulsion Laboratory (JPL) Hacked for 10 Months
CVE-2018-0256 : A vulnerability in the peer-to-peer message
processing functionality of Cisco Packet Data Network
RMIT University, COSC2737 IT Infrastructure & Security
Assignment 1: Presentation Overview](https://image.slidesharecdn.com/chapteroneintroductionlearningobjectivesbeabletoconcept-221119173534-5fdf2160/85/CHAPTER-ONEIntroductionLearning-Objectives-Be-able-to-concept-docx-112-320.jpg)