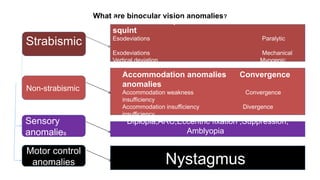
Convergence is a disjugate movement in which both eyes rotate inward so that the lines of sight intersect in front of the eyes
It allows bifoveal single vision to be maintained at any fixation distance
Remains more or less same throughout life
It does not deteriorate with increasing age