Embed presentation
Download to read offline

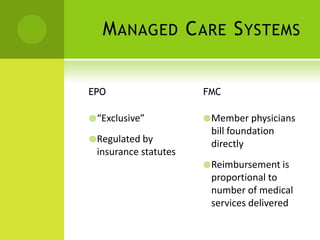
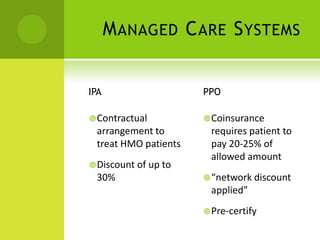
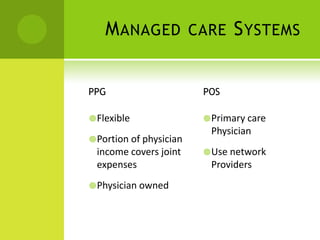

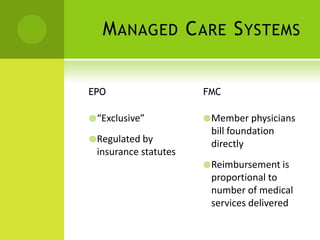
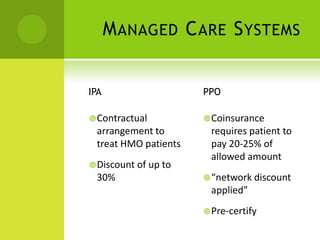
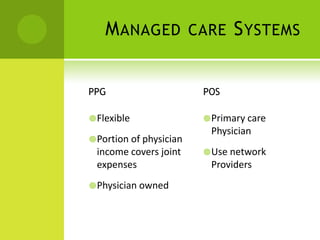
Managed care systems like HMOs, PPOs, and POS plans aim to control rising healthcare costs through mechanisms like exclusive provider networks that offer discounts, requiring precertification of treatments, and utilization review to assess efficient and appropriate use of resources. Quality Improvement Organizations work with managed care plans to ensure care meets standards through peer review and recommending actions. Prior approval is also important to confirm medically necessary services but is often unknown to patients who must always call to get it.