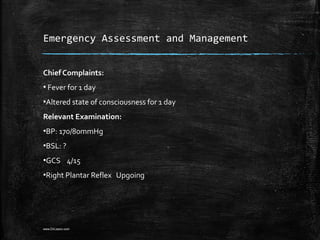
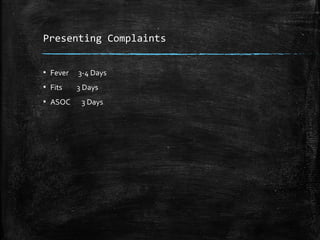
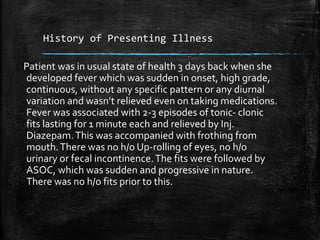
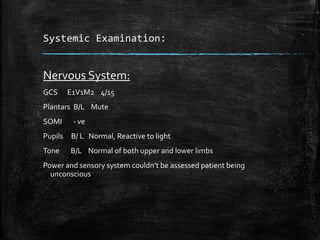
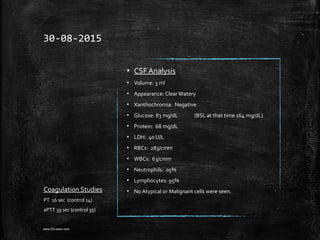
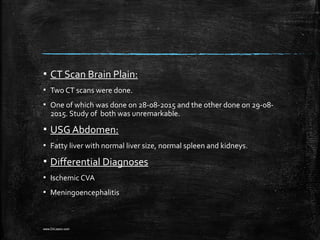
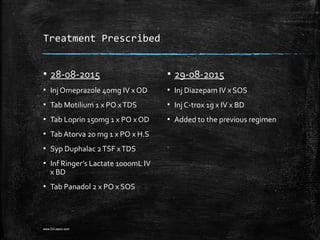
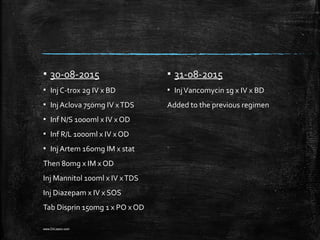
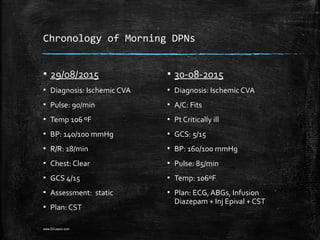
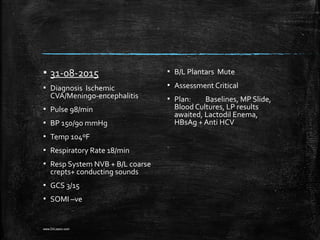
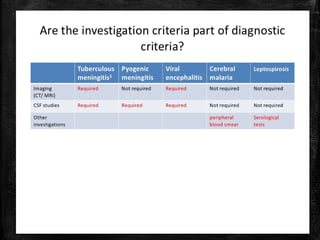
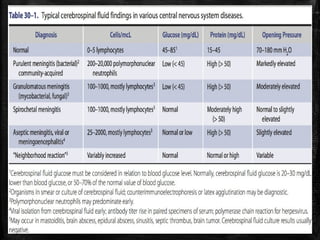
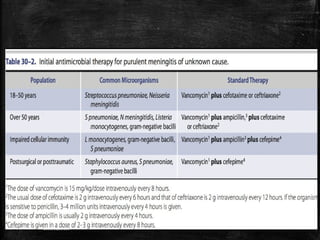
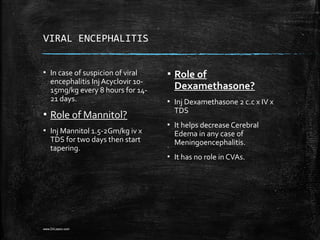
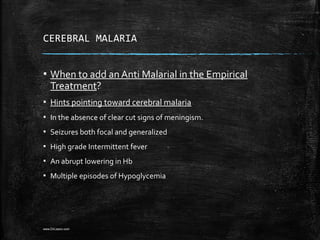
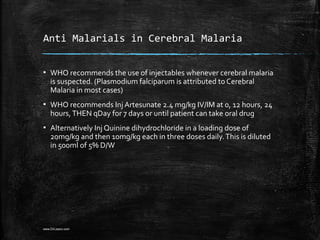
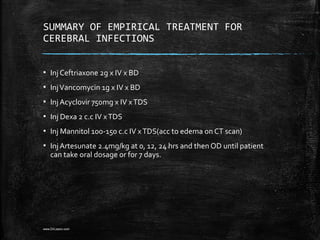
The patient presented with fever, altered consciousness, and seizures. While ischemic stroke was initially suspected, viral encephalitis or cerebral malaria should have also been considered given the association of fever. The management could have been improved by adding antiviral medication like acyclovir for possible viral encephalitis or anti-malarial drugs like artesunate for potential cerebral malaria. Dexamethasone and mannitol were also warranted to treat any cerebral edema from meningoencephalitis. Overall, a broader differential diagnosis and more comprehensive empirical antimicrobial therapy could have optimized treatment for this patient.