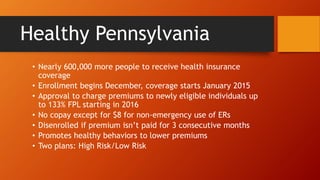
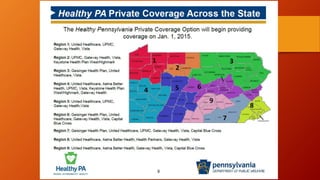
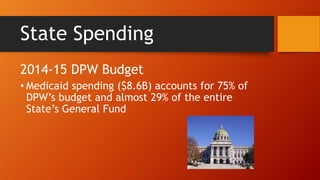
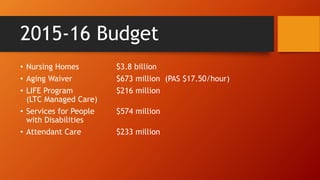
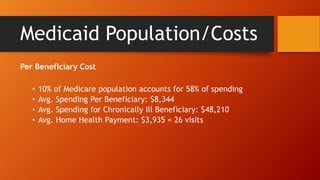
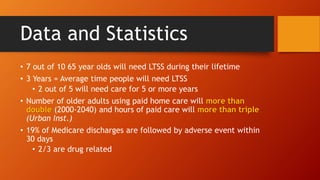
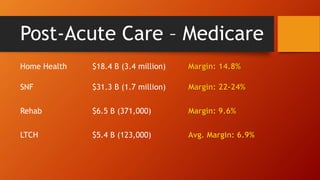
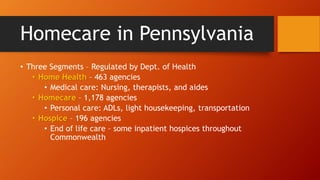
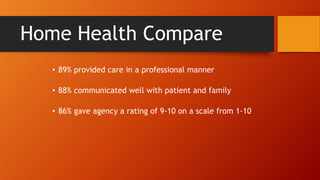
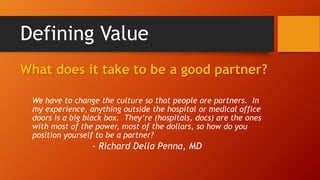
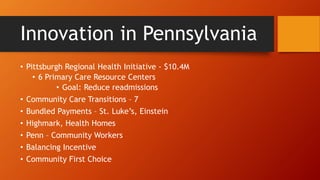
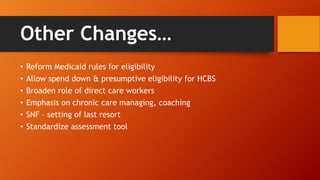
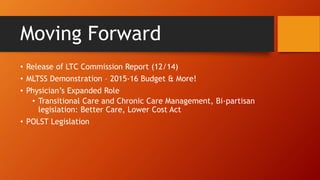
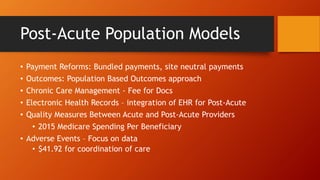
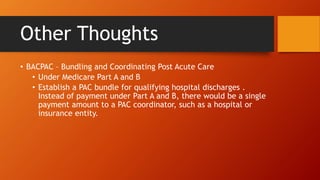
The document provides an overview of the evolving regulatory and legislative landscape for post-acute services in Pennsylvania, highlighting significant changes in healthcare coverage and spending, particularly concerning Medicaid. It outlines initiatives aimed at improving care coordination, enhancing data sharing among providers, and addressing the needs of an aging population through technological and structural reform. Additionally, the text discusses the importance of partnerships in the healthcare system and the financial challenges faced by various providers in adapting to these changes.