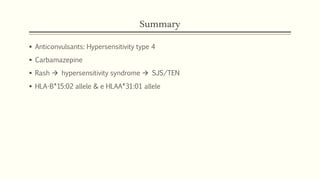
Carbamazepine is an anticonvulsant primarily used to treat epilepsy but also neuropathic pain and psychiatric disorders. It has a hypersensitivity risk of up to 10% presenting as a skin rash, but sometimes causing more severe reactions like hypersensitivity syndrome (HSS), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN). HSS is a severe adverse drug reaction affecting multiple organs with considerable morbidity and mortality. Genetic factors like the HLA-B*15:02 and HLA-A*31:01 alleles may predispose patients to carbamazepine hypersensitivity reactions.