This document provides a summary and analysis of CVS Health Corporation. It analyzes CVS Health's financial performance, the pharmacy benefits industry, and CVS Health's competition. Key points include:
- CVS Health has experienced strong financial growth but relies heavily on high-priced specialty drugs for revenue. Mergers and acquisitions could help expand its services.
- The pharmacy benefits industry faces changes from healthcare reform like value-based care. Increased regulation also poses risks.
- CVS Health is a market leader but faces intense competition on pricing and convenience. It aims to improve public health through initiatives like tobacco cessation.


![Nguyen, Leah
MBA Capstone
4
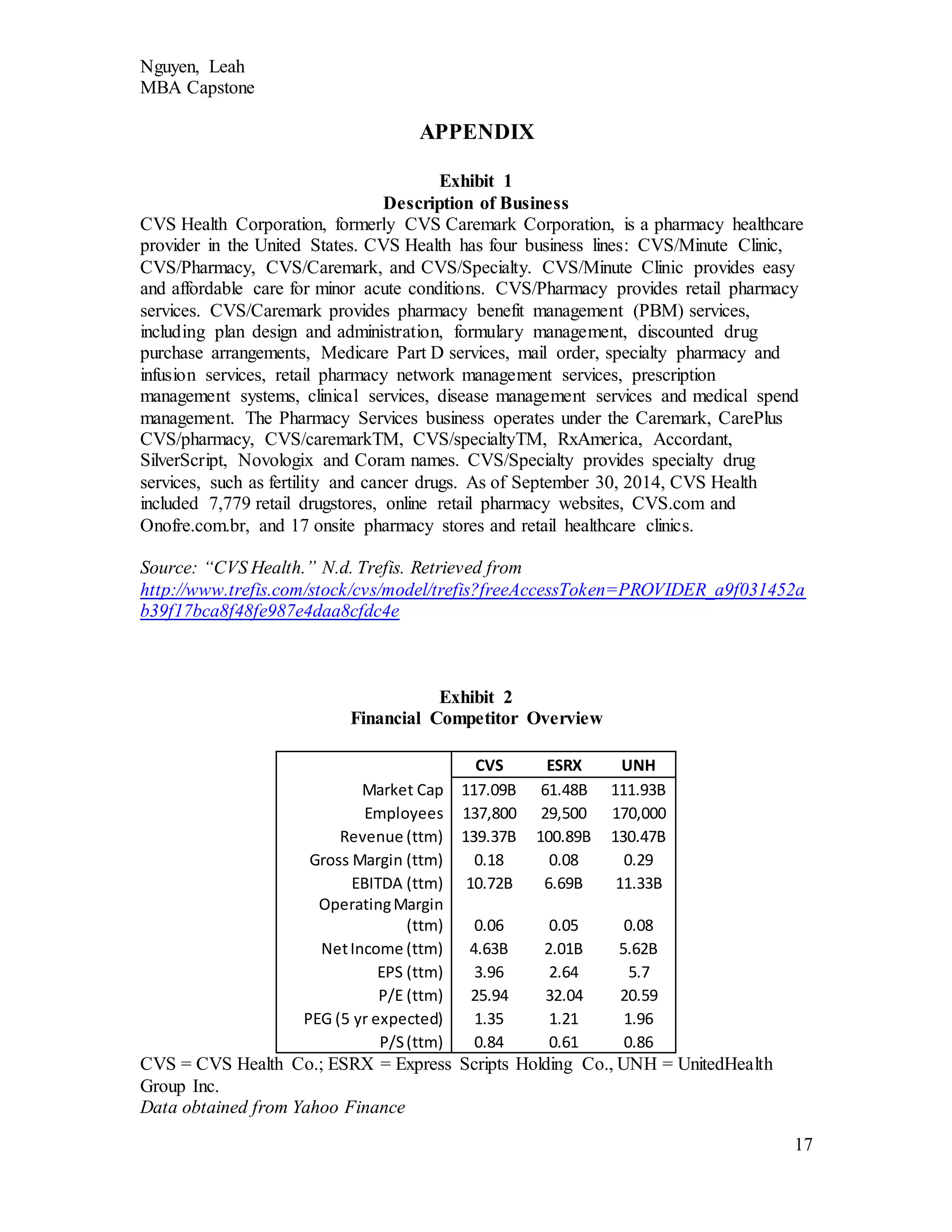
Scripts works with drug and equipment distribution, consulting, and case management. A
brief comparison of the three companies can be seen in Exhibit 2.
CVS Health has many financial strengths. They are a well-diversified company
with four different business lines: CVS/minute clinic, CVS/pharmacy, CVS/caremark,
and CVS/specialty. Each of these provides a separate function while working cohesively
to achieve improved patient and consumer well-being. For example, certain specialty
drugs are no longer being processed through the pharmacy store but instead through their
mail order capacity. While this lowered basis points for the pharmacy, it increased overall
revenues compared to prescription volumes due to the high price of specialty drugs
(“CVS Health Reports Strong Profits,” 2015). These high-priced specialty drugs are
growing in demand. In the last quarter, revenues for these drugs increased nearly 22
percent to $23.9 billion (Associated Press, 2015). CVS Health also benefitted from the
increase in patient access due to the ACA, as more patients were being treated and filling
prescriptions. UnitedHealth and Express Scripts also saw this increase, and this increase
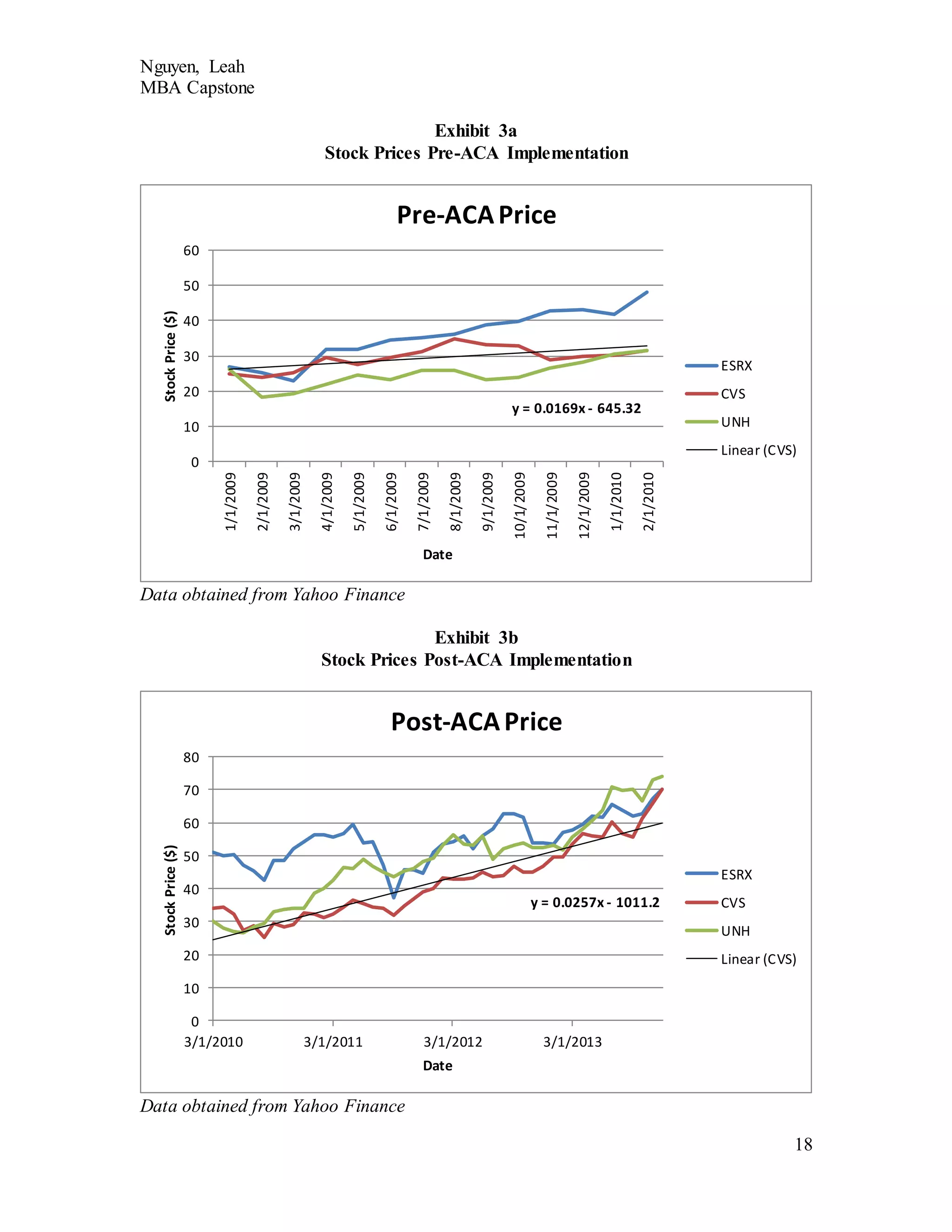
in value was translated into stock price. Exhibits 3a and 3b show the difference in rate of
stock price increase before and after the ACA of CVS Health, Express Scripts, and
UnitedHealth. As illustrated, the rate nearly doubles after implementation of the ACA.
In the last quarter, earnings rose 4 percent despite the “anticipated blow” from the
termination of sales from tobacco products (Associated Press, 2015). For the total year of
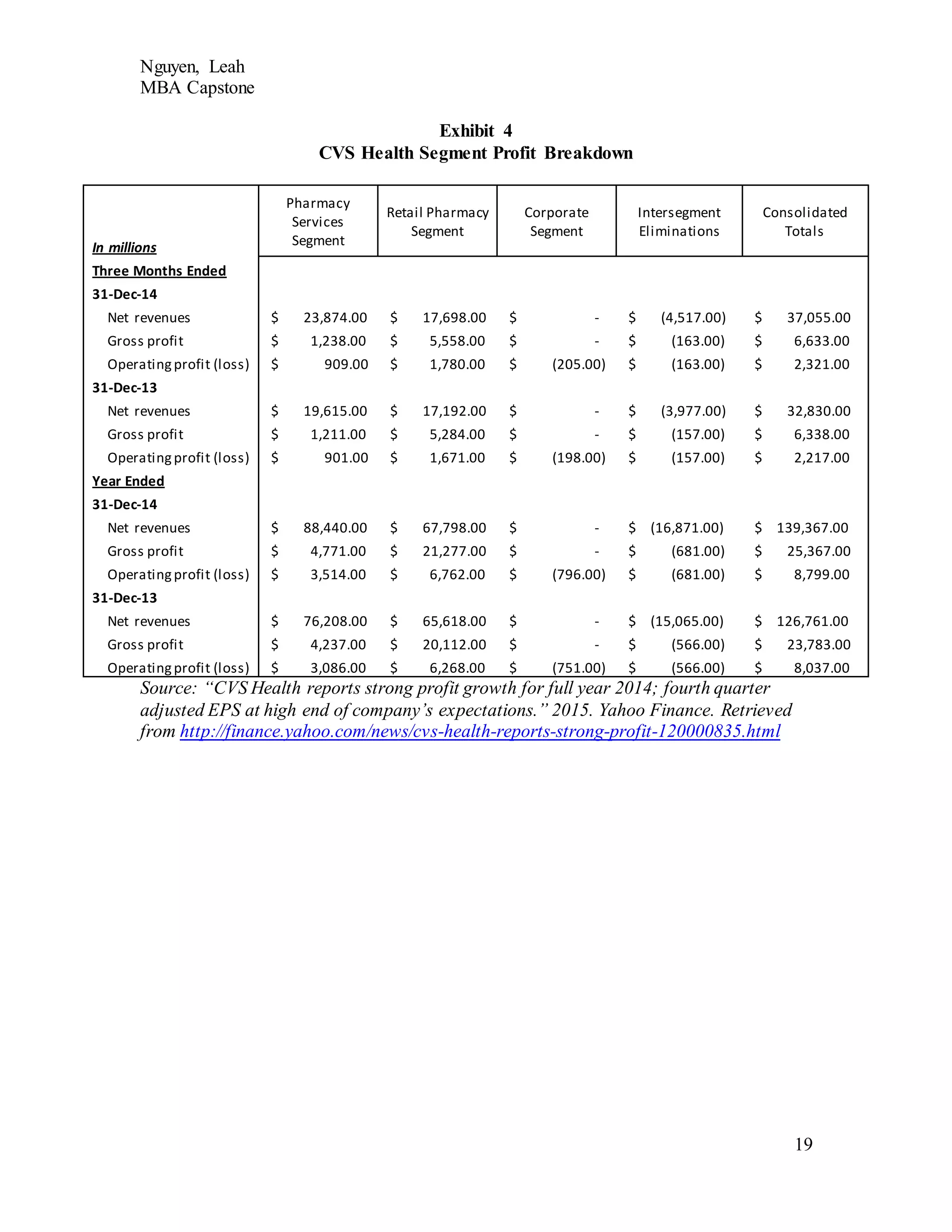
2014, net revenues increased 9.9 percent to a record $139.4 billion [Exhibit 4] and CVS
Health generated free cash flow of $6.5 billion and cash flow from operations of $8.1
billion (“CVS Health Reports Strong Profits,” 2015). This cash flow “exceeded” CVS](https://image.slidesharecdn.com/4c402d77-1ec5-4859-8f45-3962a3bbaa85-150702220338-lva1-app6892/75/Capstone-PaperFinal-5-2048.jpg)
![Nguyen, Leah
MBA Capstone
6
There are several opportunities for CVS Health to take advantage. As has
happened throughout the industry, mergers and acquisitions of other PBMs and pharmacy
services companies is common. When UnitedHealth acquired Catamaran Corporation, it
became the third-largest pharmacy benefit manager with a market share of 20 percent
(“What the UnitedHealth-Catamaran Deal Means,” 2015). Before this, CVS Health and
Express Scripts controlled about 50 percent of the PBM market, with Express Scripts
filling over one billion prescriptions annually. The acquisition of Catamaran brings
UnitedHealth’s estimated fulfillment of prescriptions to mirror that of Express Scripts at a
billion. CVS Health has acquired several smaller companies in the past, such as Coram in
2013, a specialty infusion services unit, and Long Drug Stores in 2008 (Townsend,
2013). To maintain its market share, CVS Health should continue exploring these
opportunities to expand their expertise and services to provide lower-cost and more
accessible care.
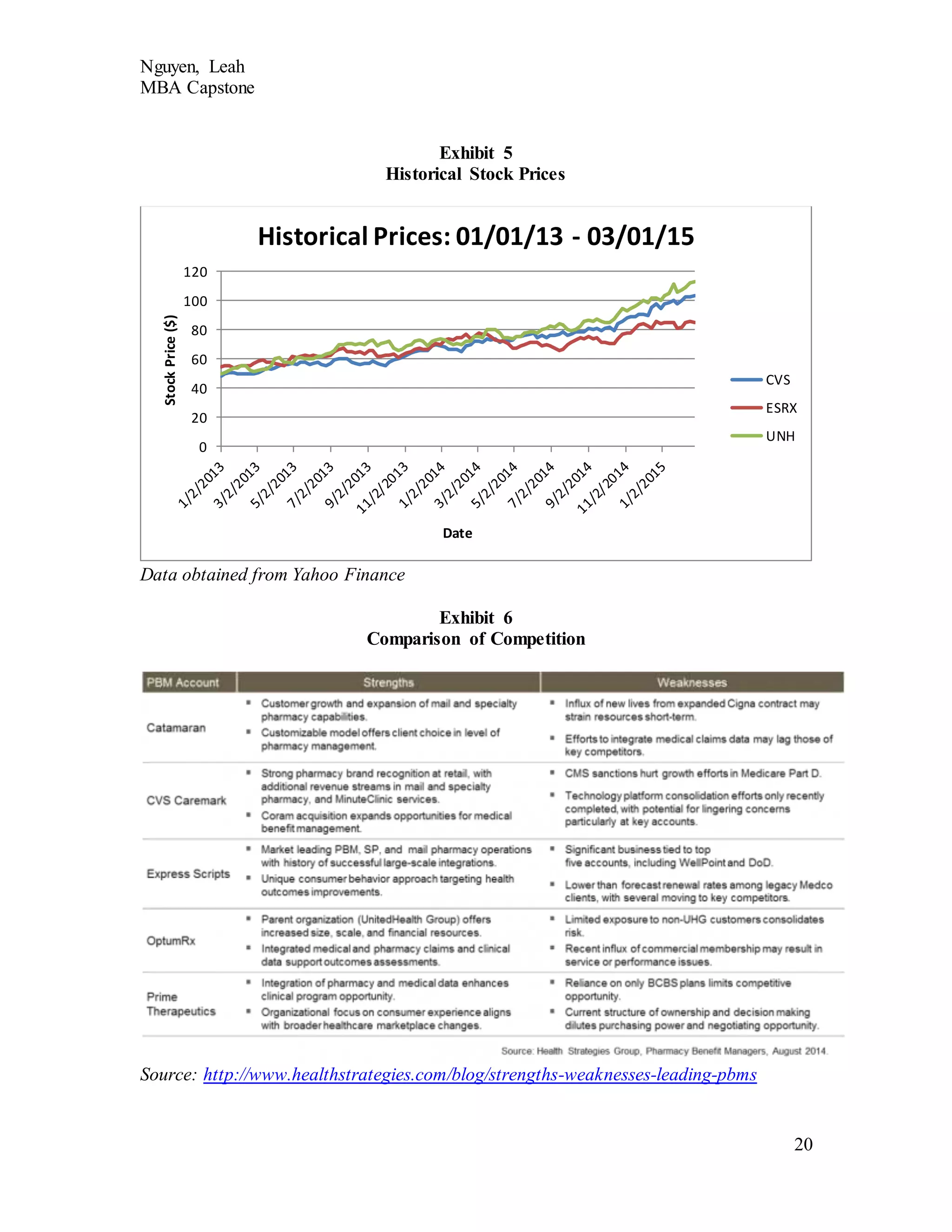
A final opportunity for CVS Health is to improve their stock price. Despite the
recent financial successes, CVS Health is not as strong as UnitedHealth. They are doing
much better than Express Scripts, but there is always opportunity for improvement
[Exhibit 5]. This could be achieved through increasing the value of the company to
increase demand for shares as well as buy back some of their shares to reduce the supply
of shares available.
Being a player in the healthcare system does not come without risks or threats.
CVS Health, UnitedHealth, and Express Scripts are threatened by litigation. As these
companies grow larger through acquisitions, the competition is effectively consolidated
into a few major players that have the potential for anti-trust law violations. Settlements](https://image.slidesharecdn.com/4c402d77-1ec5-4859-8f45-3962a3bbaa85-150702220338-lva1-app6892/75/Capstone-PaperFinal-7-2048.jpg)
![Nguyen, Leah
MBA Capstone
12
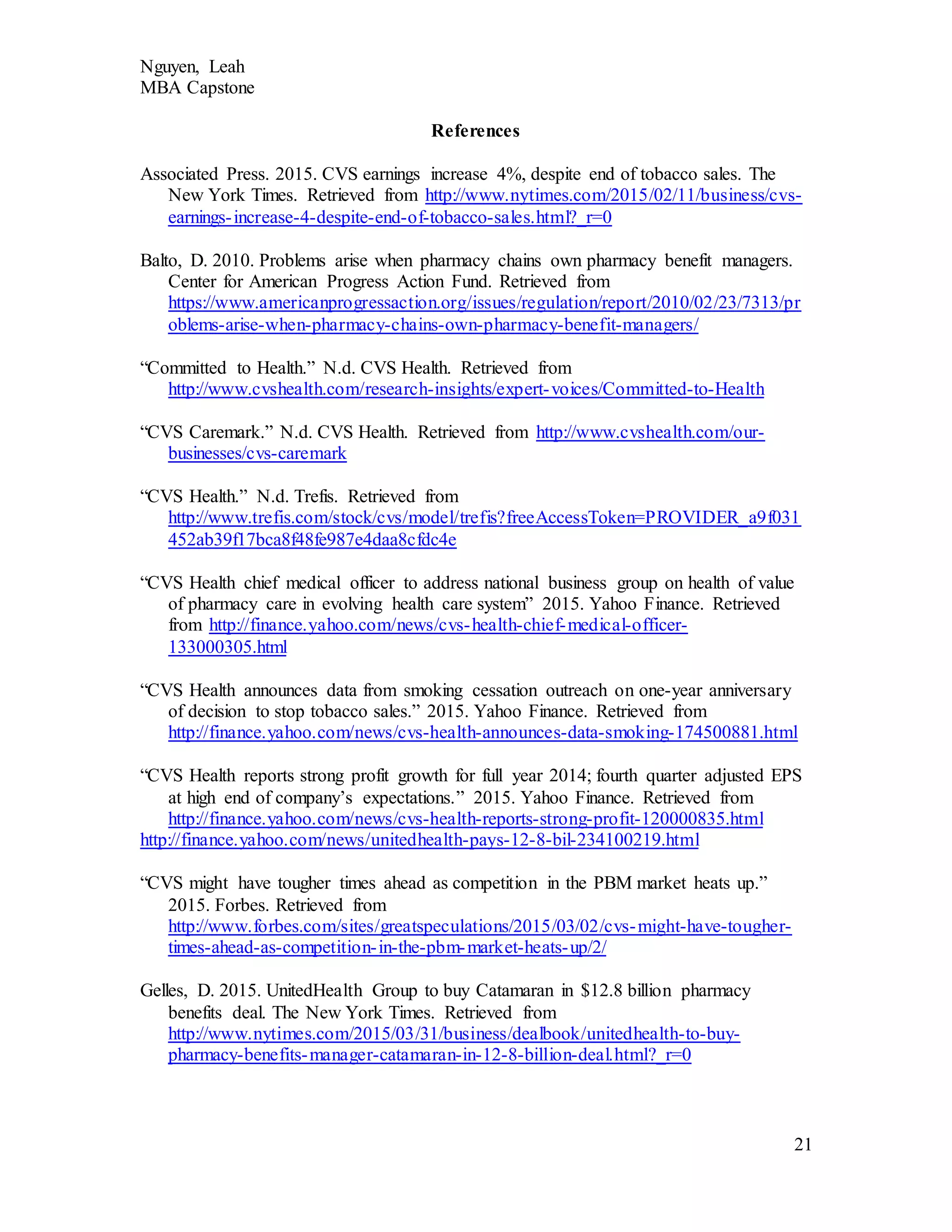
Exhibit 6 for an overall comparison – note that Catamaran and OptumRx are now part of
UnitedHealth].
In the face of these competitors, CVS Health has many strengths. By
eliminating tobacco products from their stores, they created a very strong marketing tool.
This well publicized action gave CVS Health a platform to further prove their
commitment to health and well-being. CVS Health’s Eileen Boone explained that
“cigarettes simply have no place in a setting where health care is delivered” and that
many conditions that pharmacies help manage are made worse by smoking (Kanani,
2014). In conjunction with this, they introduced a tobacco cessation program for their
customers that combined medication and coaching from the pharmacy staff. They also
rebranded from CVS Caremark to CVS Health in 2014 to emphasize their dedication to
health. CVS Health also has a separate Corporate Social Responsibility department that
operates several philanthropic efforts under the platform “Prescription for a Better
World.” These efforts prove to the public that CVS Health is committed to their mission
and may convince consumers to use their services instead.
Another strength of CVS Health’s is their proprietary technology. One use of
this technology is in the retail pharmacy. It is able to perform safety checks, interaction
screening, and substitutions for generic and brand drugs (“CVS Health,” n.d.). Their
technology also has the ability to deliver patient-specific information directly to EHRs to
the patients’ providers, integrating even more into the PCMH model. This improves
quality of care and safety for their patients.
The major weakness of CVS Health is the significant power that comes with
major acquisitions, like those of their competitors. As mentioned in the financial analysis,](https://image.slidesharecdn.com/4c402d77-1ec5-4859-8f45-3962a3bbaa85-150702220338-lva1-app6892/75/Capstone-PaperFinal-13-2048.jpg)