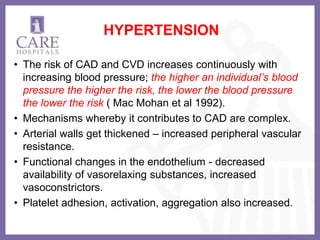
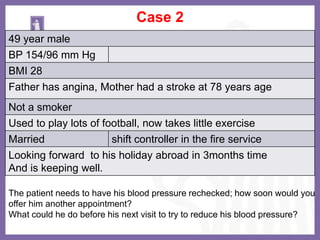
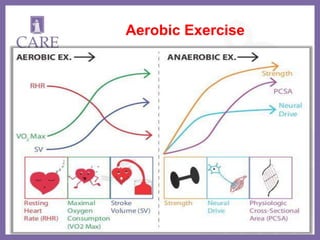
This document discusses primary prevention of coronary artery disease. It defines primary prevention as action taken prior to disease onset to prevent disease from ever occurring, through screening, health exams, and modifying risk factors. The document outlines modifiable risk factors for heart disease like smoking, hypertension, diabetes, obesity, and high cholesterol. It provides strategies for risk factor modification including lifestyle changes like a healthy diet, exercise, and medication if needed. The goal of primary prevention is to tailor therapy to high risk individuals before significant disease develops.