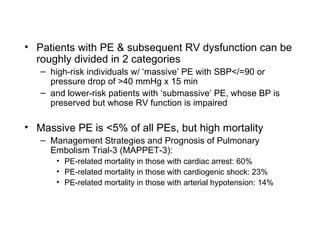
The document discusses the management of massive pulmonary embolism (PE), which is defined as PE with systolic blood pressure ≤90 mmHg or a pressure drop of >40 mmHg for 15 minutes. Initial treatment involves oxygen, pain control, and cautious IV fluids. If PE is confirmed on CT or echocardiogram, thrombolytics are given if not contraindicated. For patients who fail or cannot receive thrombolytics, catheter-based thrombolysis or surgical embolectomy are options. The risks and diagnostic alternatives of renal failure are also covered.