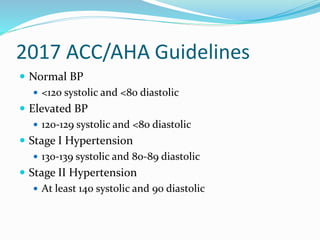
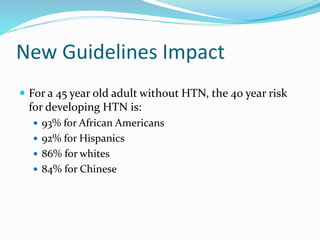
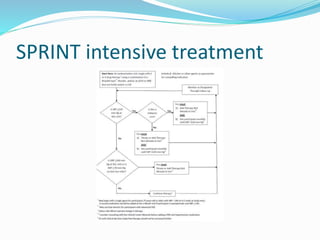
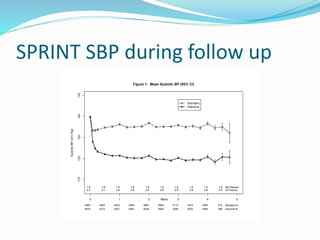
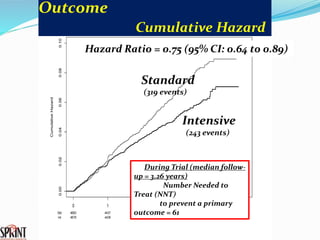
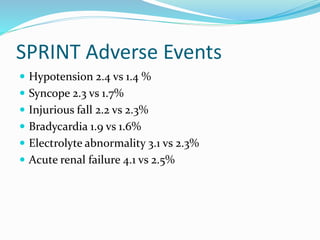
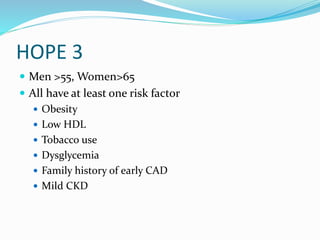
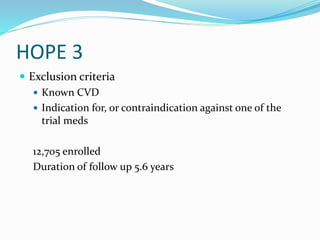
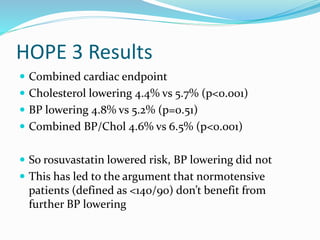
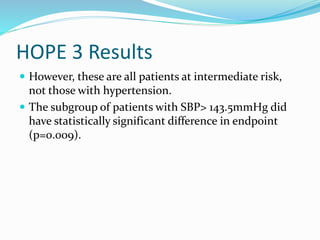
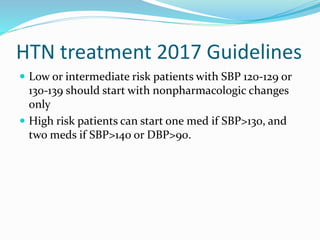
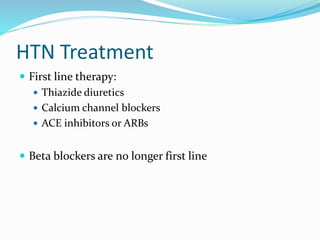
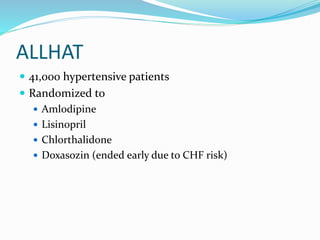
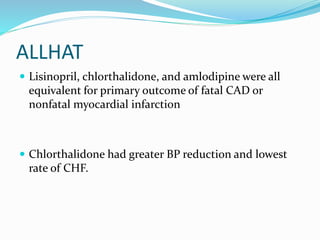
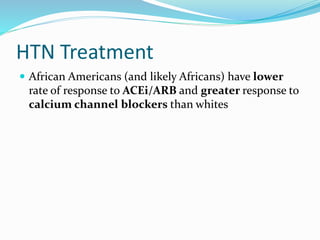
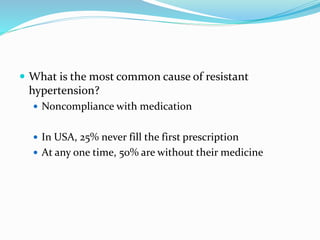
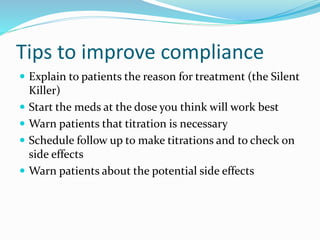
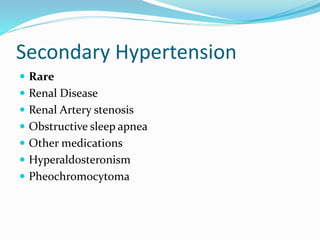
This document discusses guidelines for diagnosing and treating hypertension. It summarizes findings from the SPRINT and HOPE-3 trials regarding blood pressure targets. The SPRINT trial found that treating systolic blood pressure to under 120 mmHg reduced cardiovascular risks more than treating to under 140 mmHg. However, the HOPE-3 trial found statin therapy reduced risk more than blood pressure medication alone in intermediate-risk patients. The document provides recommendations on lifestyle changes, medication options, special patient populations, and evaluating treatment resistance and secondary causes of hypertension.