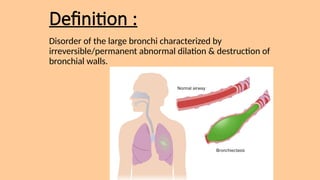
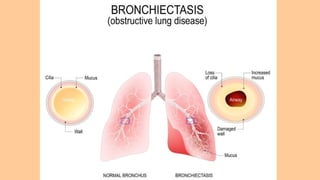
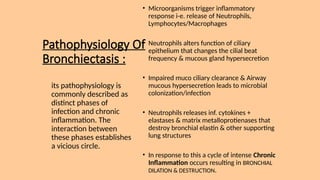
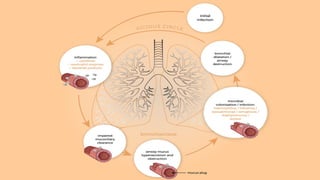
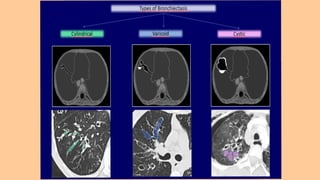
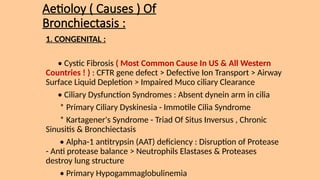
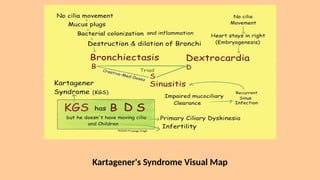
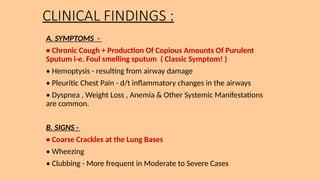
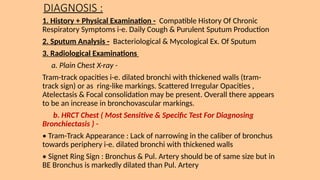
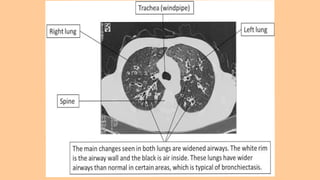
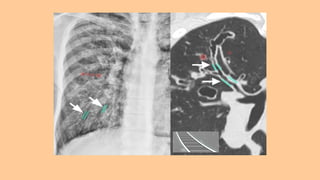
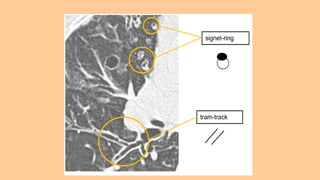
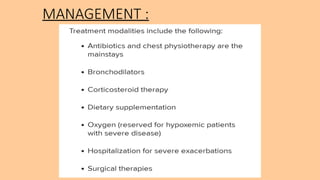
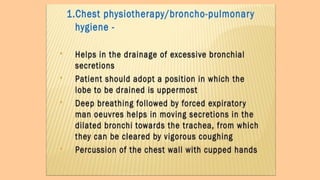
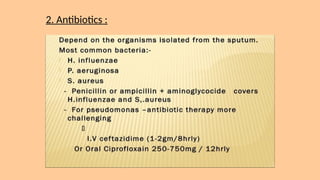
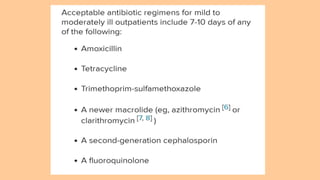
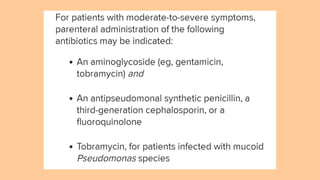
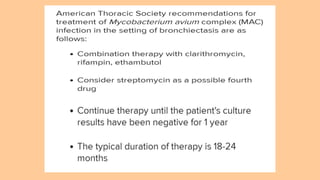
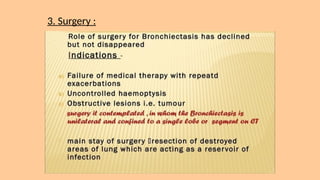
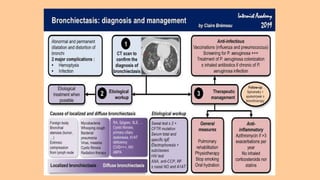
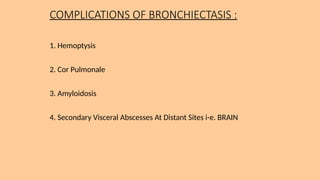
Bronchiectasis is an obstructive lung disease characterized by irreversible dilation and destruction of bronchial walls, primarily caused by chronic inflammation and infections. It can be classified into cylindrical, varicose, and saccular forms, with common causes including congenital conditions like cystic fibrosis and acquired conditions such as tuberculosis. Diagnosis involves a combination of patient history, sputum analysis, radiological examinations, and pulmonary function tests, while management may include antibiotics and surgery.