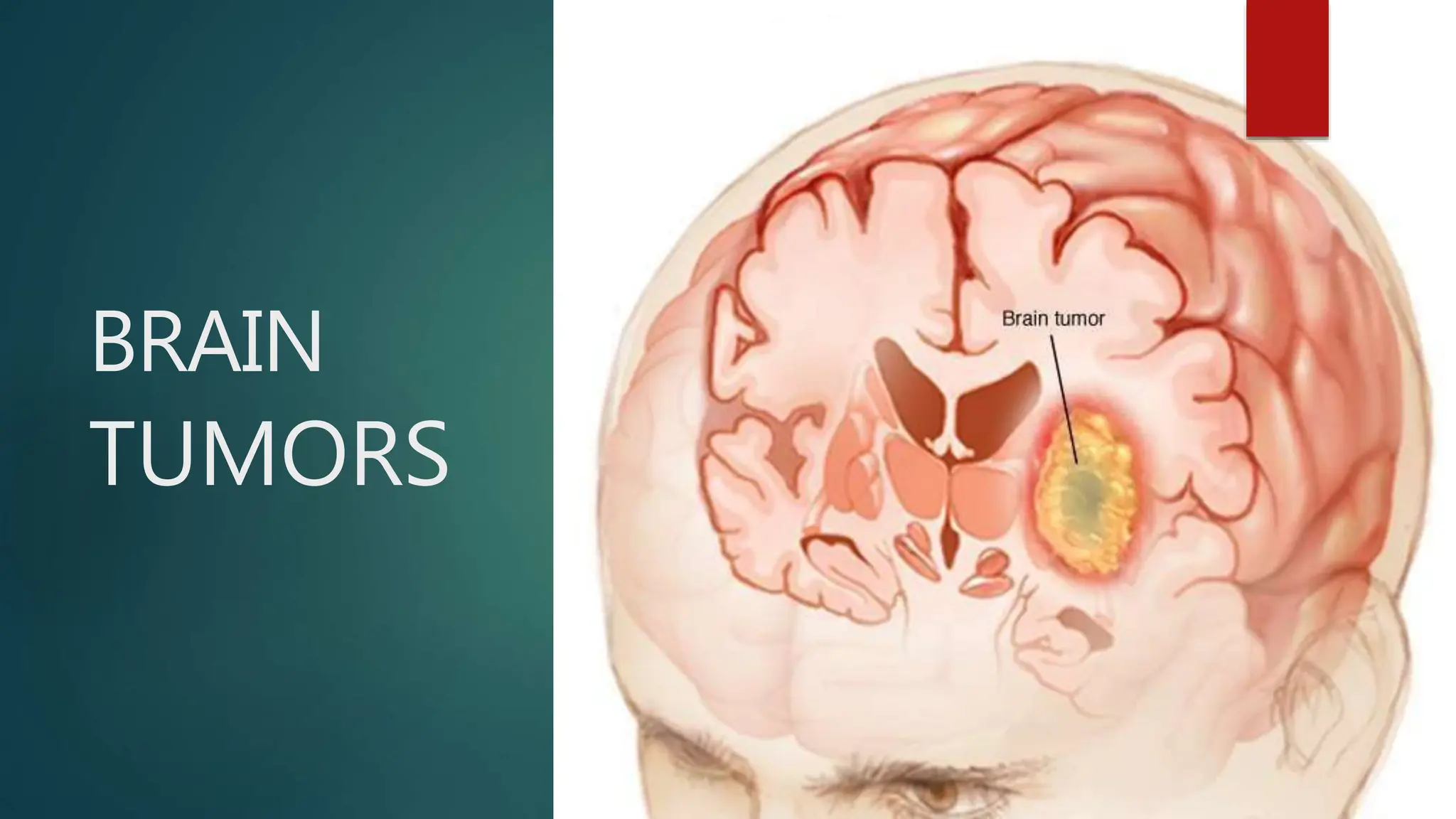
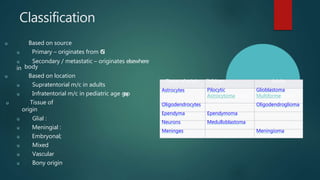
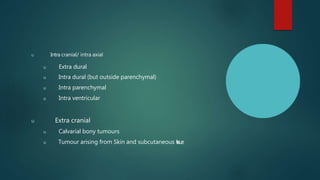
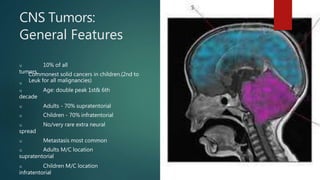
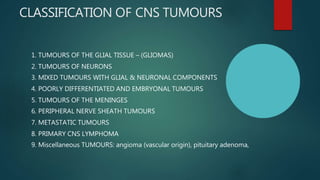
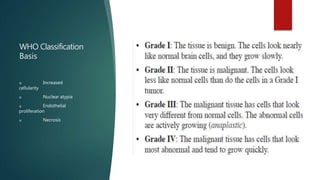
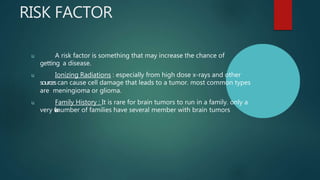
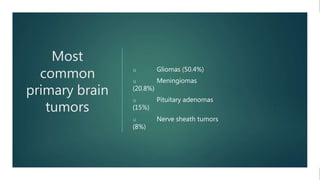
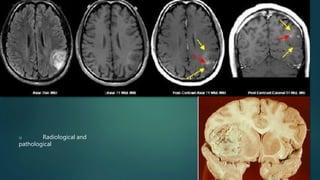
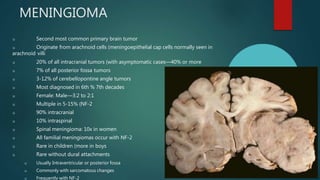
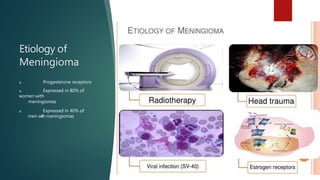
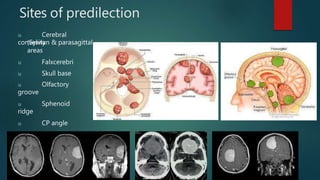
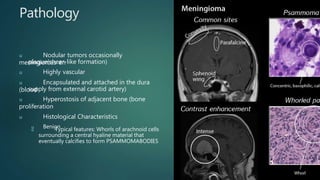
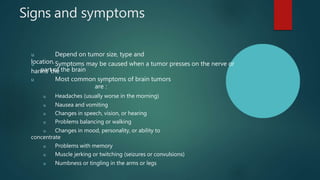
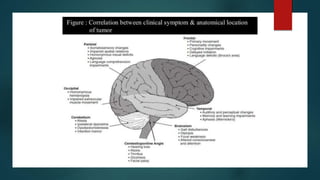
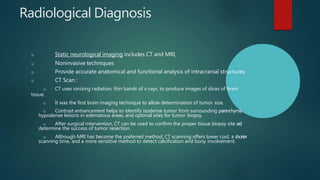
Brain tumors are abnormal masses due to uncontrolled cell growth, categorized into benign and malignant types, originating from various cell types and locations within the central nervous system. Common primary brain tumors include gliomas, meningiomas, and pituitary adenomas, with specific symptoms such as headaches, seizures, and cognitive changes indicating their presence. Diagnosis relies on clinical assessments and imaging techniques like CT and MRI, which aid in determining tumor size and location.