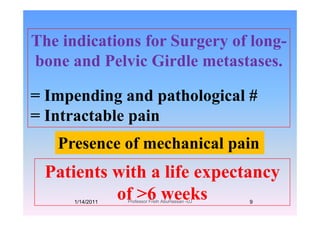
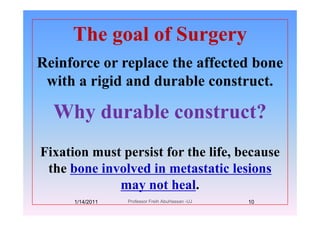
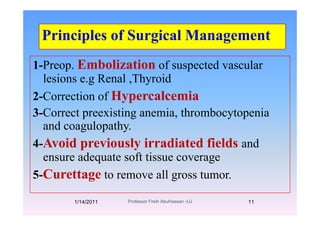
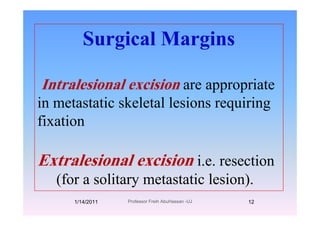
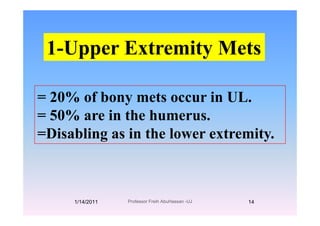
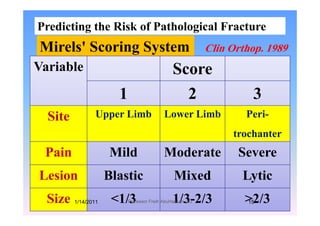
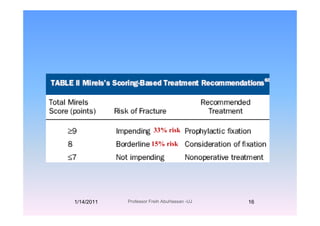
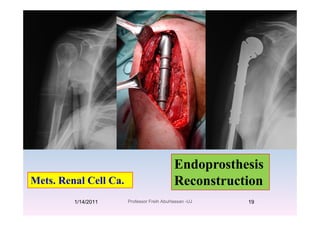
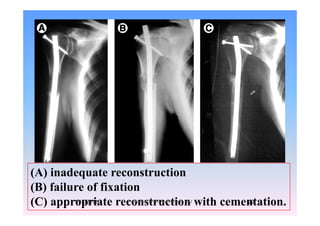
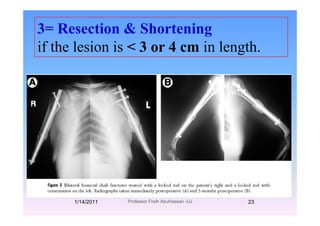
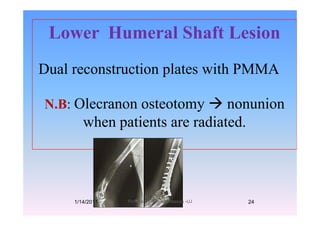
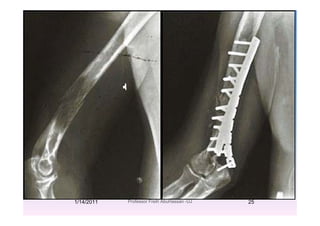
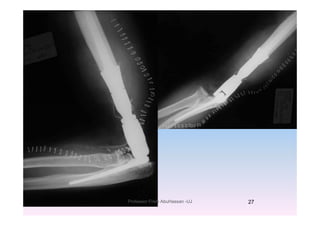
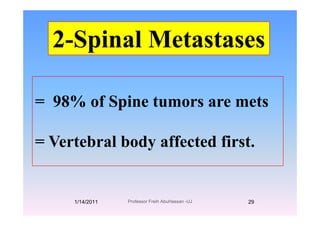
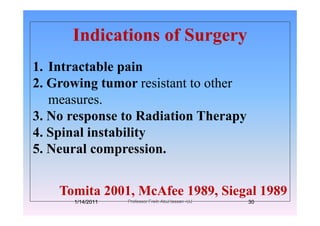
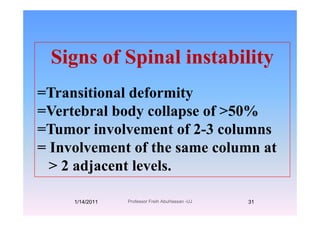
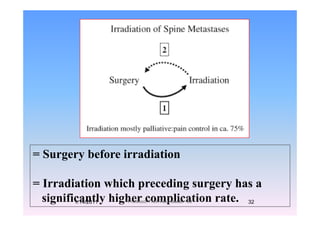
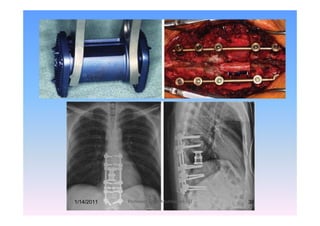
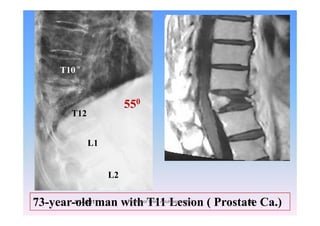
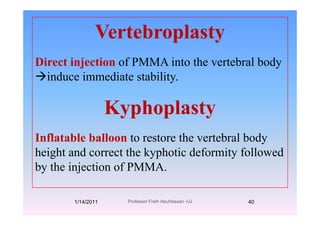
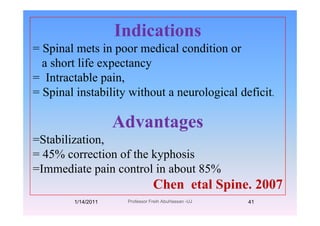
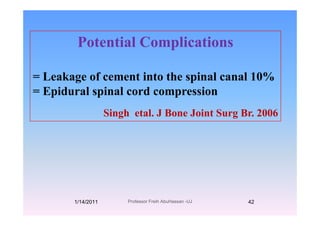
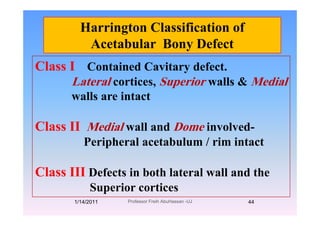
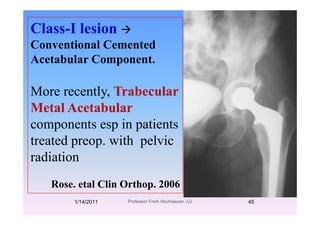
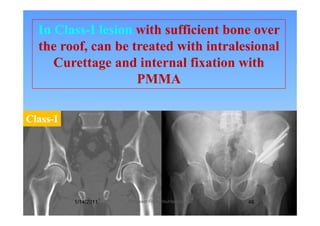
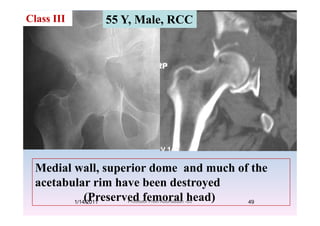
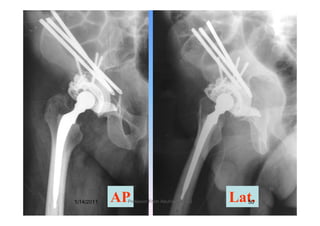
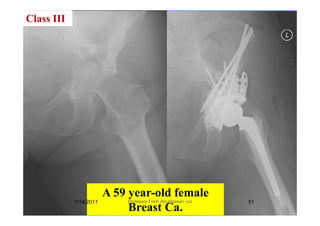
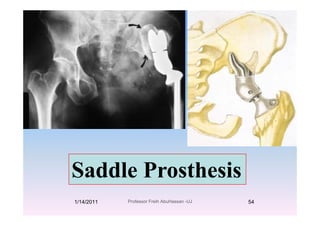
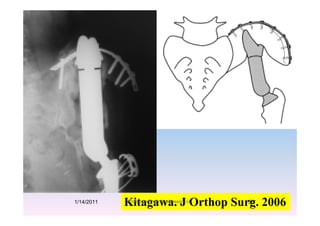
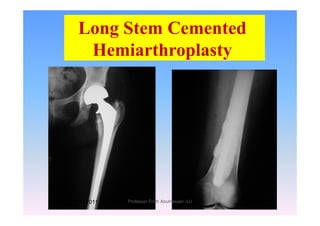
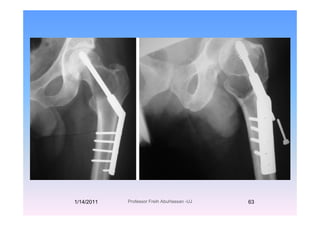
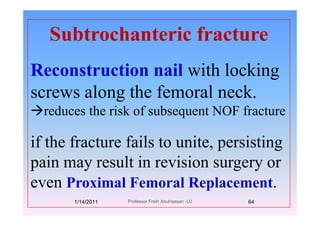
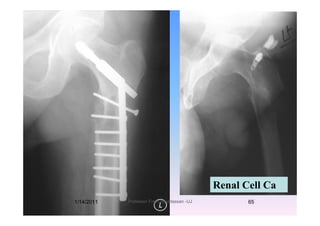
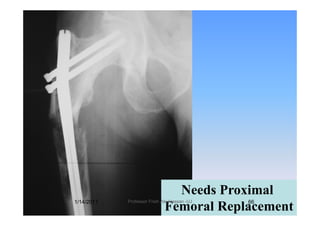
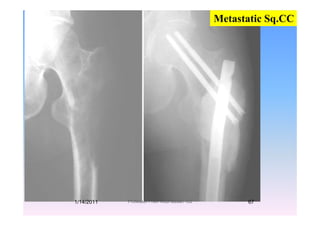
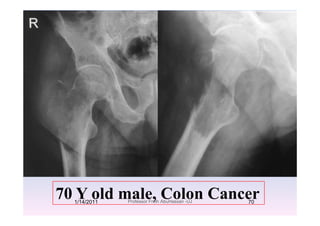
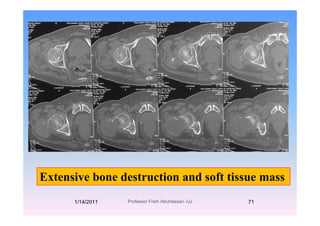
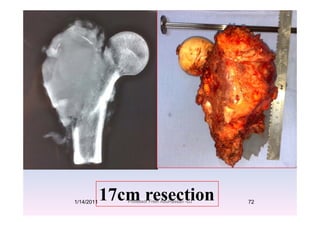
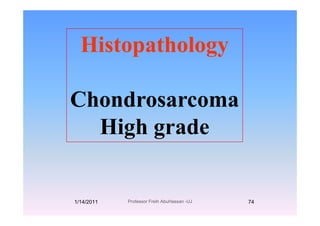
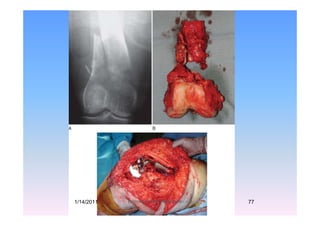
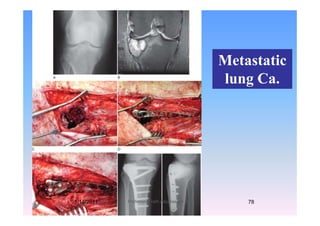
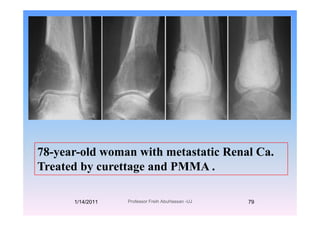
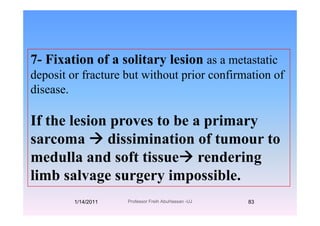
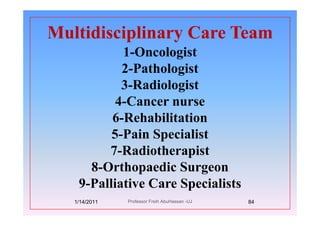
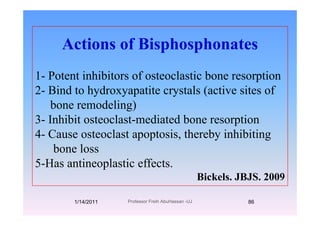
The document discusses the challenges and management of bone metastasis, emphasizing its increasing prevalence and the need for orthopedic planning for durable fixation. It highlights common errors in diagnosis and surgical management that hinder patient outcomes and outlines various management strategies, including surgical indications and techniques for different metastasis types. Additionally, it addresses the goals of surgery, preoperative considerations, and complications in specific cases such as spinal and periacetabular lesions.