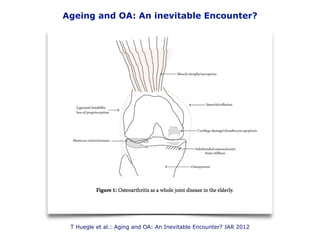
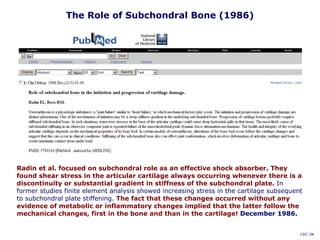
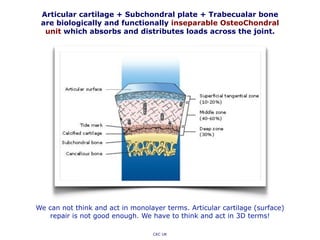
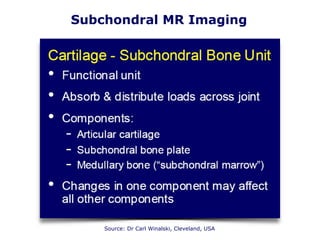
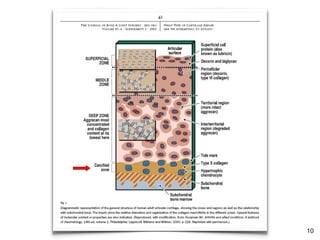
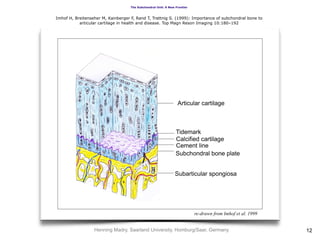
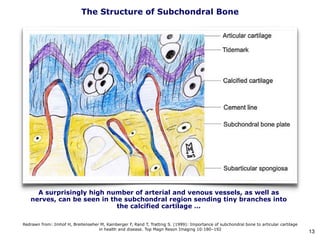
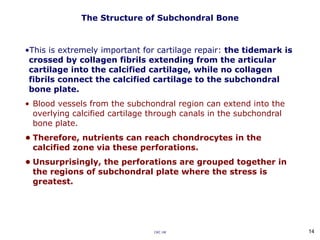
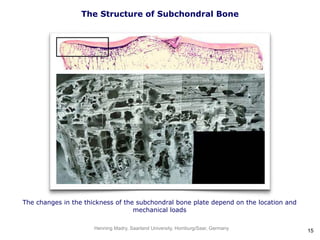
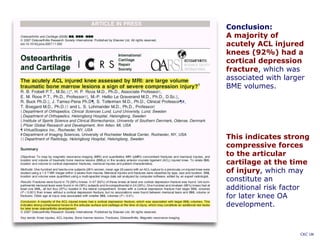
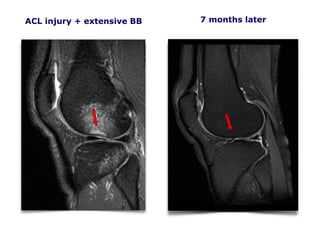
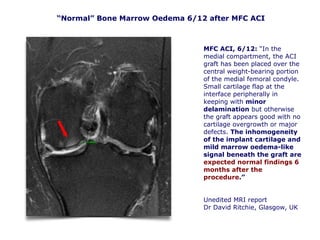
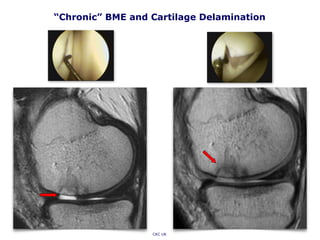
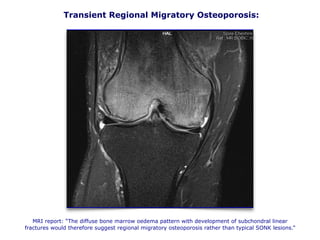
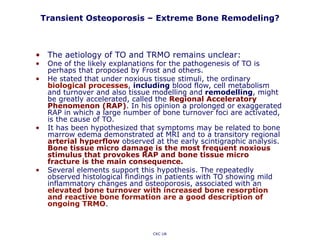
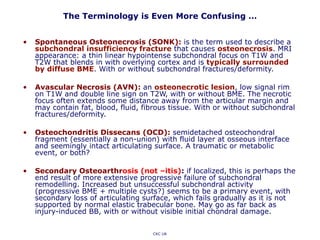
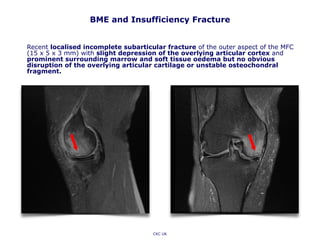
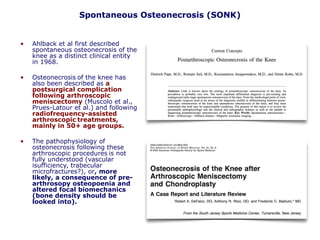
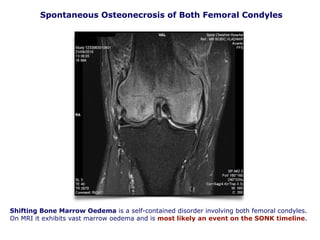
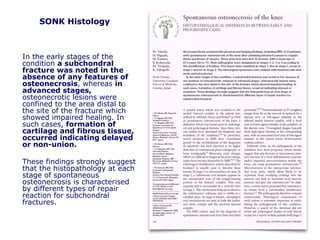
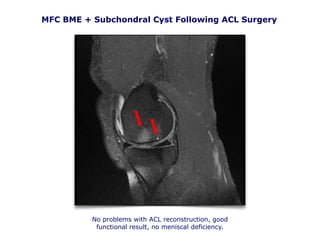
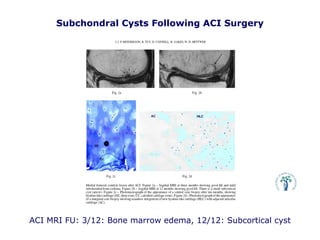
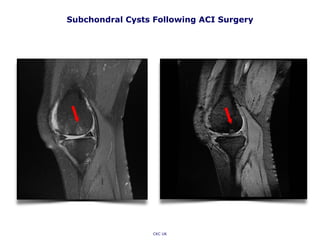
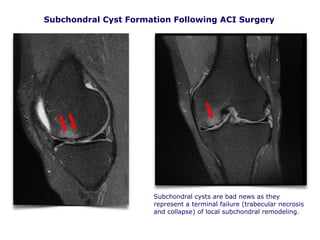
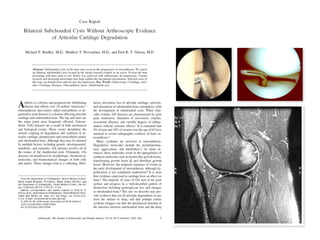
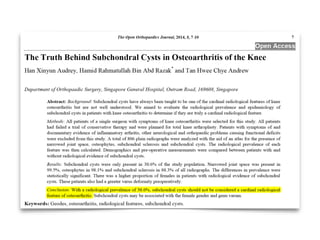
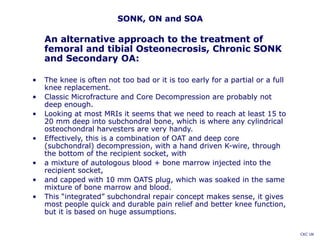
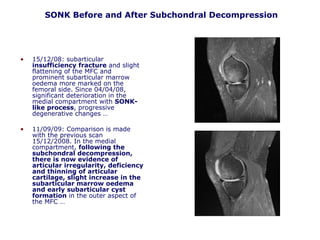
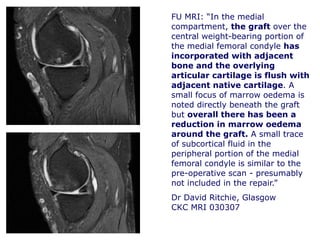
This document summarizes a presentation on subchondral bone and cartilage aging. It discusses how subchondral bone and cartilage act as a single functional unit, and changes in subchondral bone can lead to stresses in overlying cartilage. While subchondral bone stiffening was thought to contribute to cartilage damage in osteoarthritis, one study found decreasing subchondral bone density and thickness with age, even as osteoarthritis increased. The terminology around subchondral bone lesions seen on MRI, like bone marrow edema, is confusing as they often represent extensive bone remodeling rather than true edema. Maintaining the integrity of the osteochondral unit may be important for cartilage repair procedures.