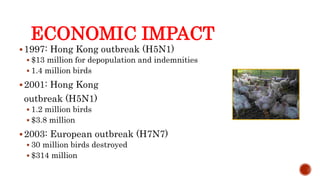
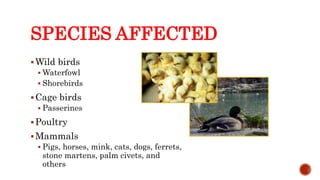
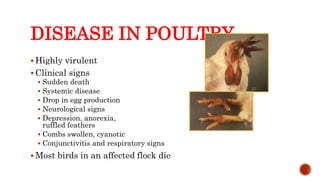
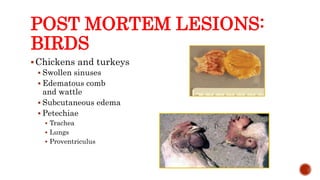
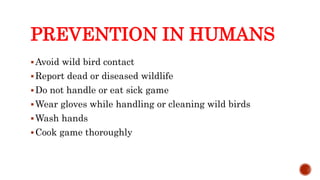
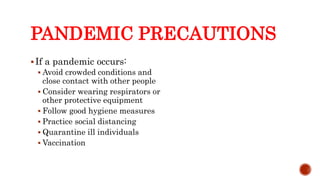
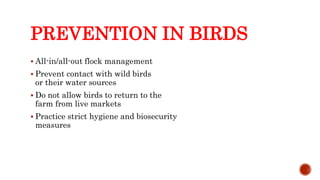
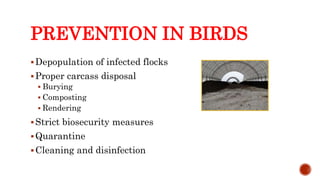
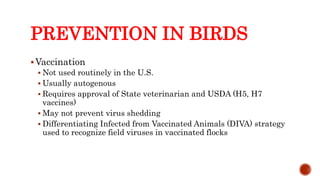
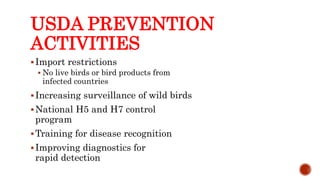
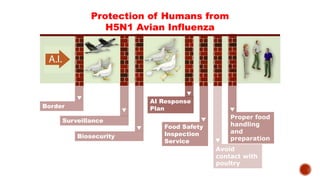
This document discusses avian influenza, including its organism classification, pathogenicity in birds, reservoirs, transmission, disease presentation, diagnosis, treatment and prevention. It covers the virus's history, epidemiology in various regions, and impacts on humans, domestic poultry, and other animal species. Key points include how the virus is transmitted between wild birds and poultry and its potential to cause pandemics if adapting to spread between humans. Prevention focuses on notification of authorities, quarantine, and hygienic practices around infected birds.