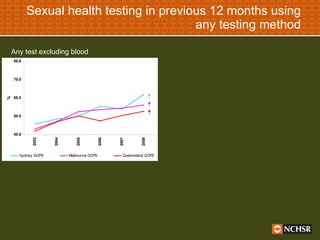
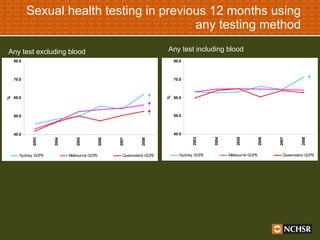
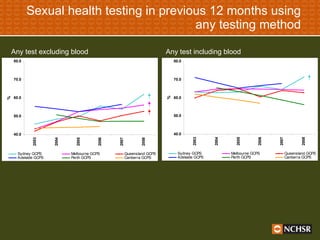
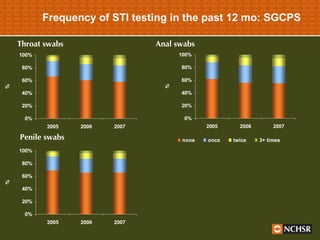
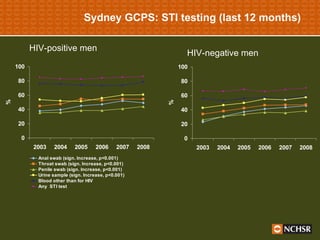
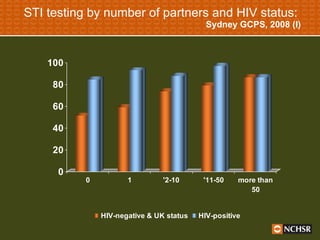
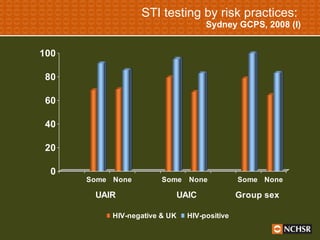
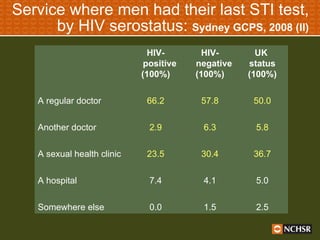
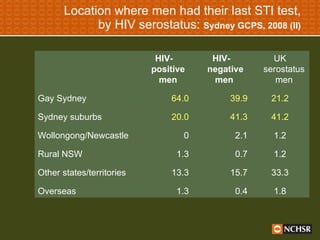
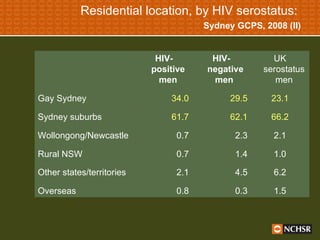
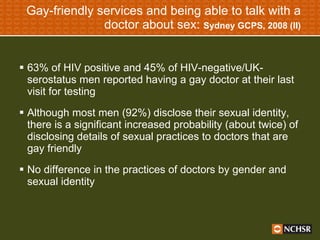
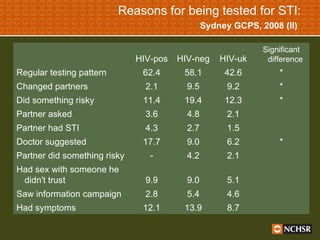
The document presents findings on sexual health testing practices and behaviors among gay men in Australia, highlighting trends in STI and HIV testing from 1998 to 2008. It emphasizes the increased frequency of testing, revealing that while most men are aware of STI prevention strategies, risky sexual behaviors persist, particularly among HIV-negative men who access gay-friendly services less frequently. Additionally, it points out the discrepancies in STI prevalence and testing behaviors based on HIV serostatus, stressing the need for improved access to testing for all men.