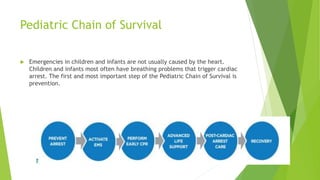
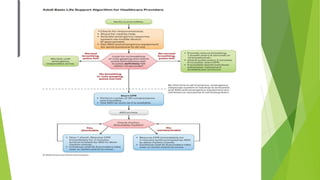
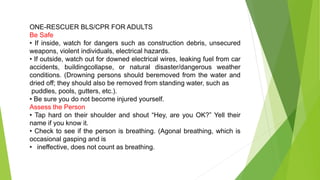
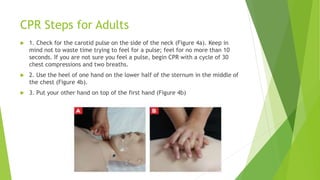
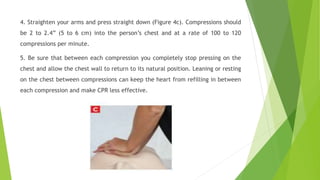
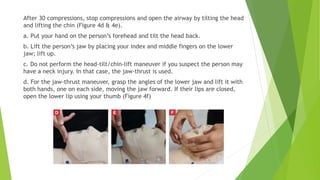
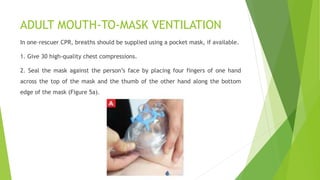
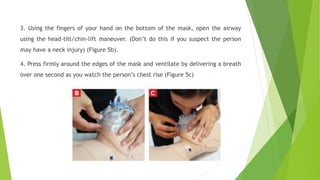
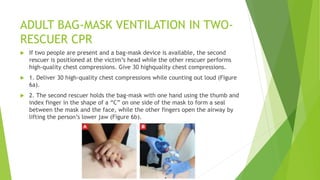
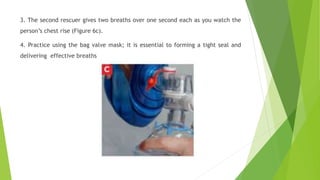
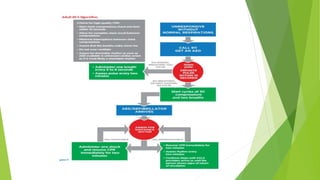
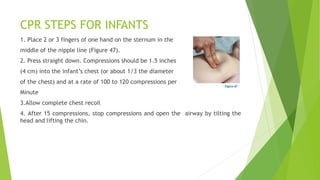
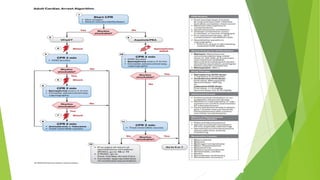
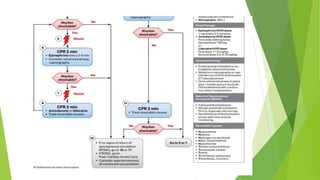
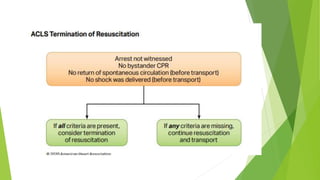
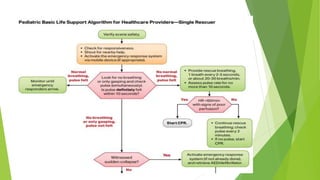
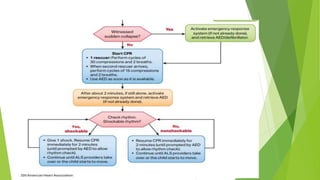
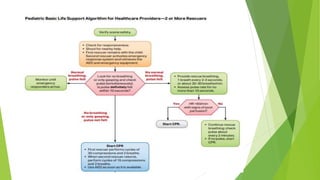
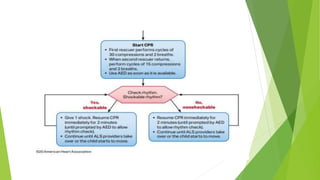
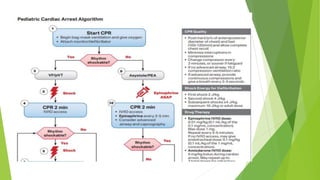
This document provides information on basic life support (BLS) techniques for adults, children, and infants. It discusses initiating the chain of survival, assessing an unresponsive person, performing chest compressions and rescue breathing, using an automated external defibrillator (AED), and two-rescuer CPR techniques. Key steps for one-rescuer BLS for adults, children, and infants are outlined, including chest compression depth and rate, head tilt/chin lift, rescue breathing, and using a pocket mask or bag valve mask for breaths.