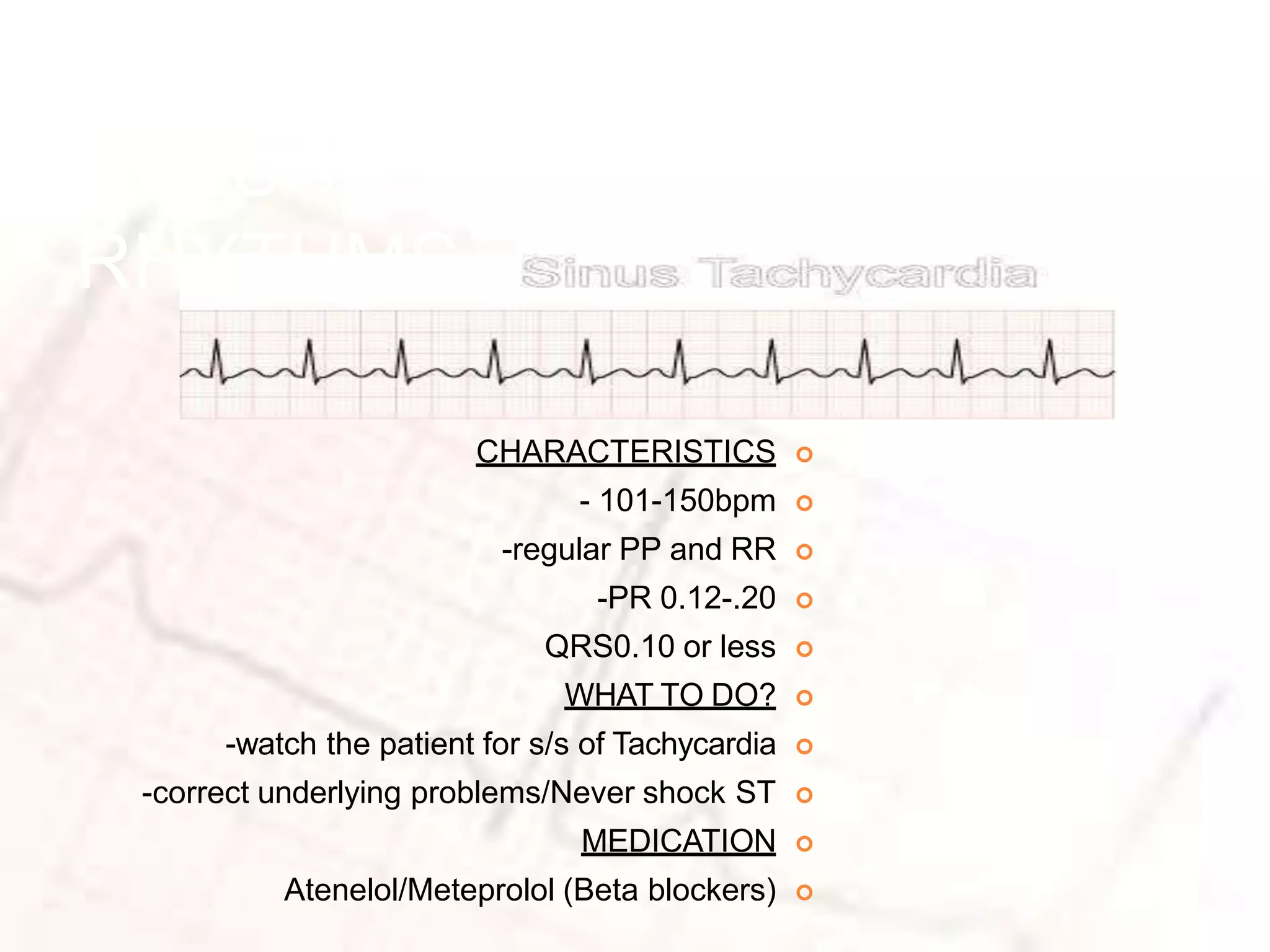
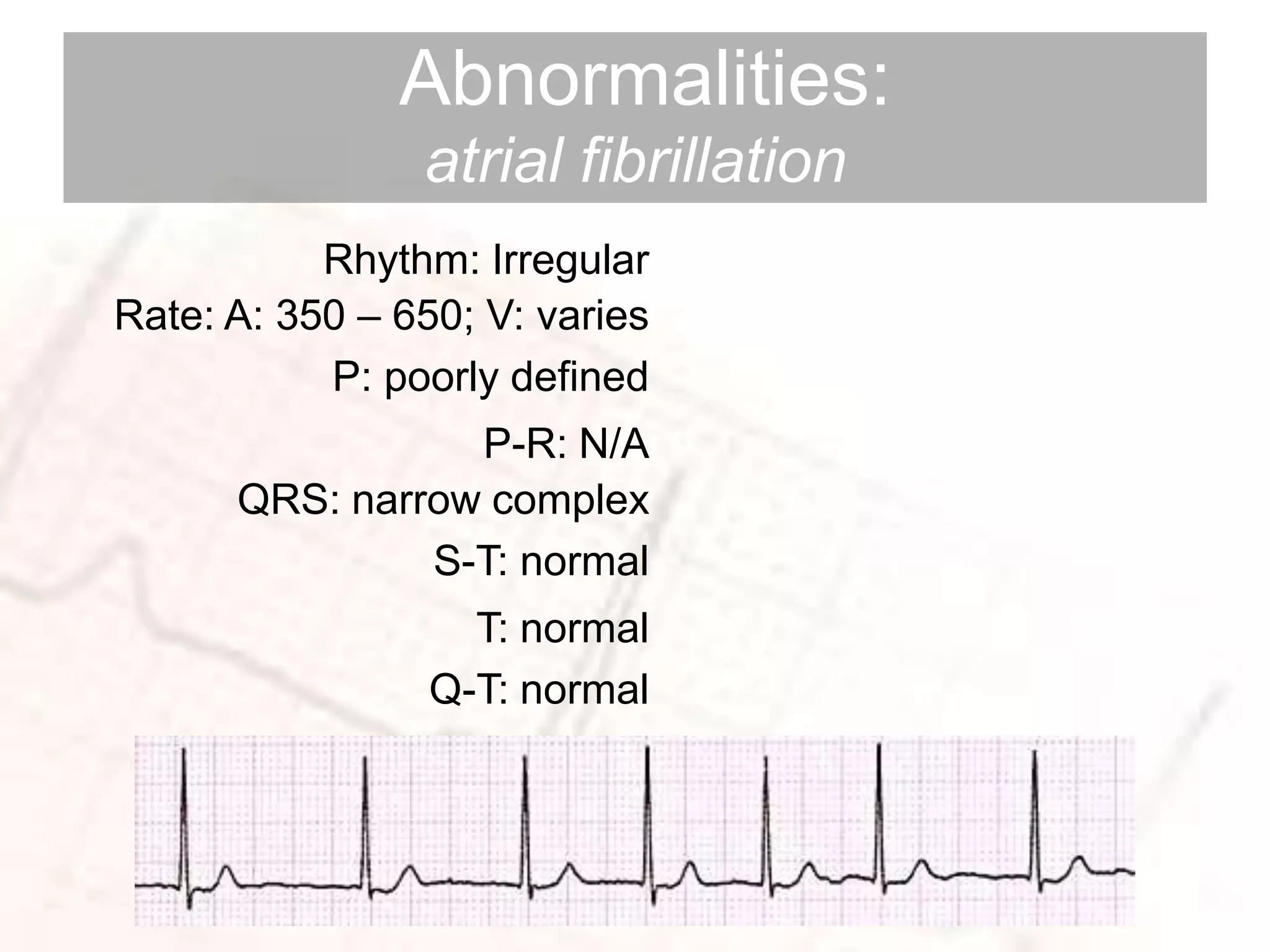
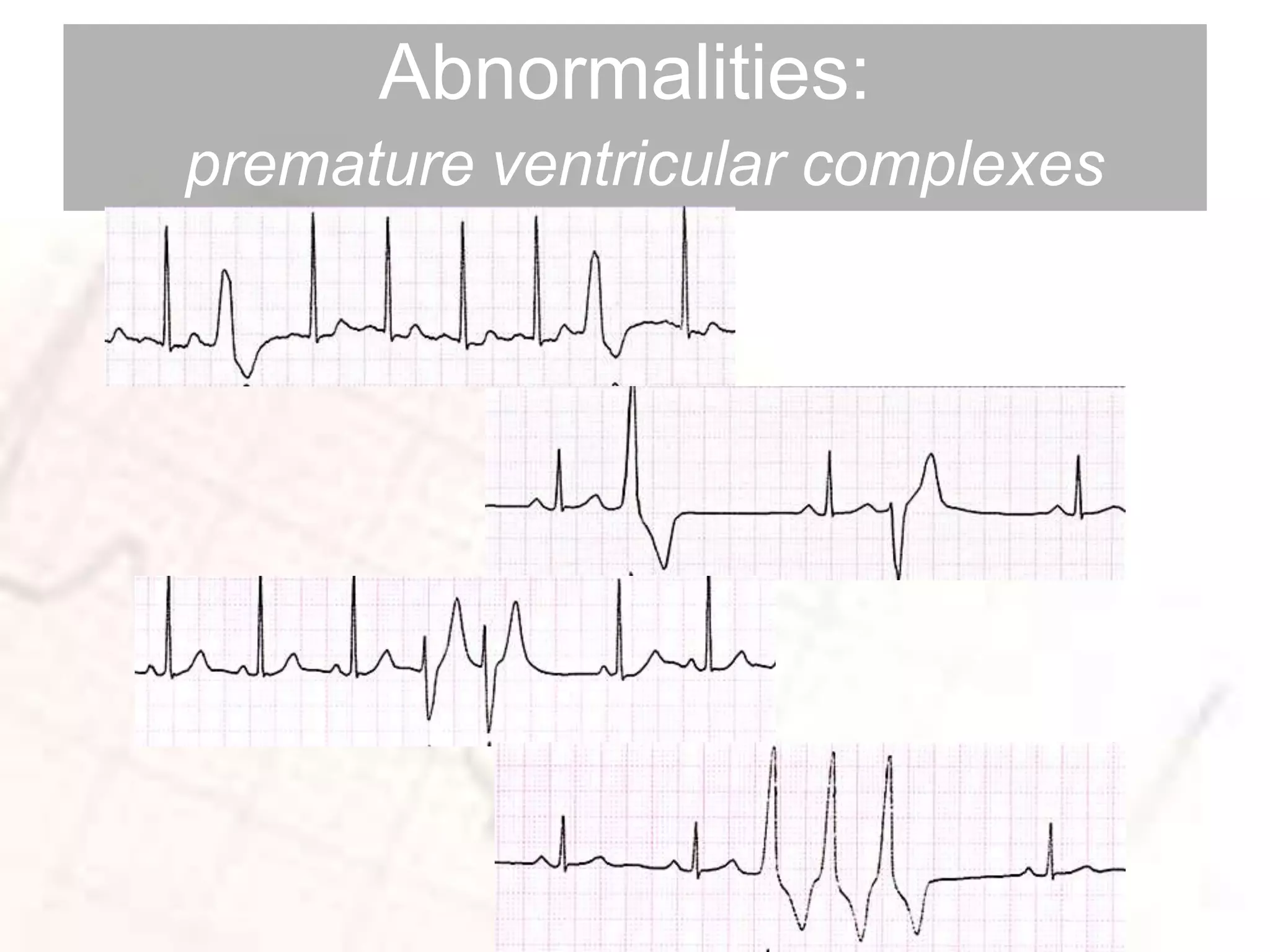
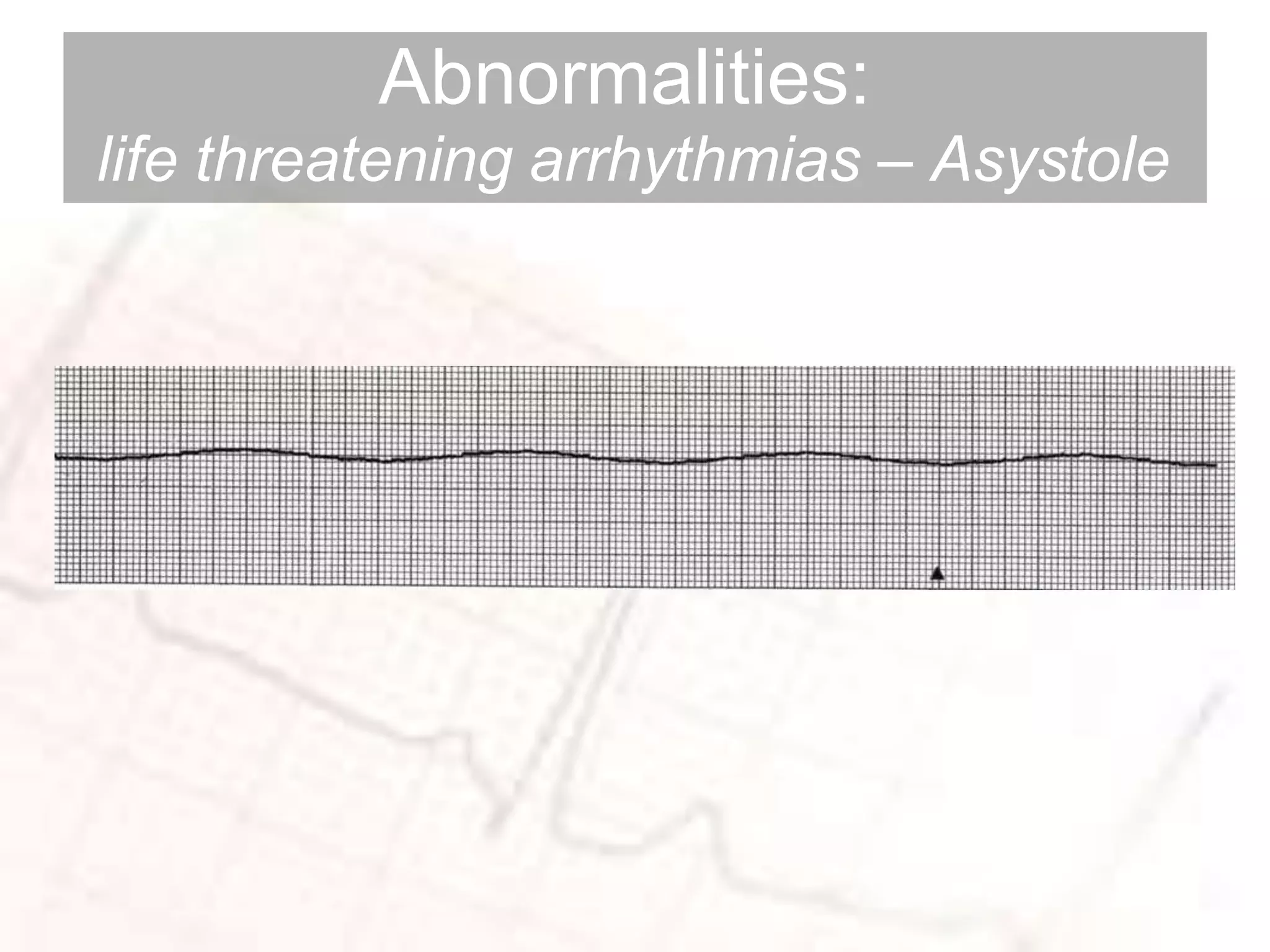
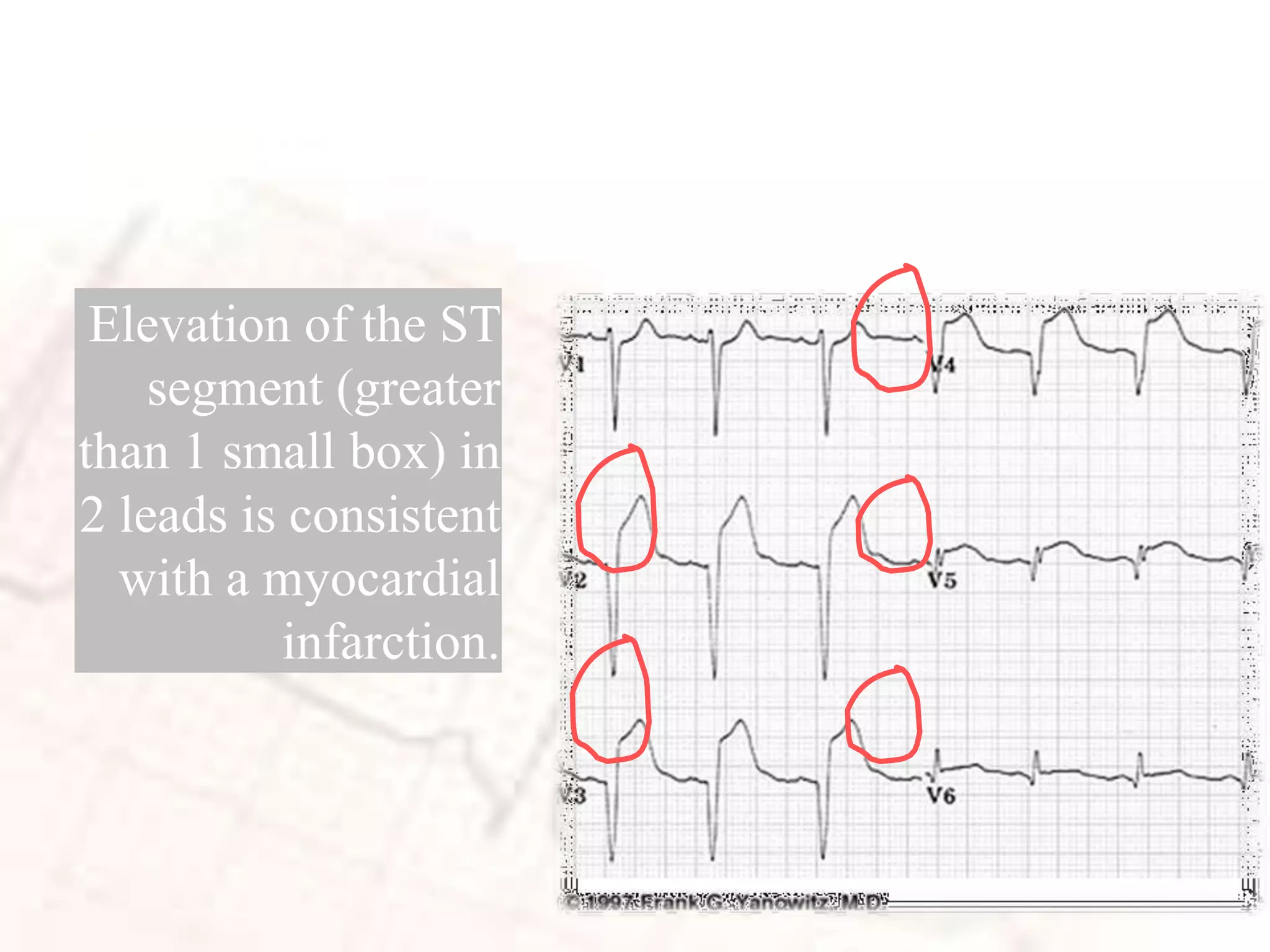
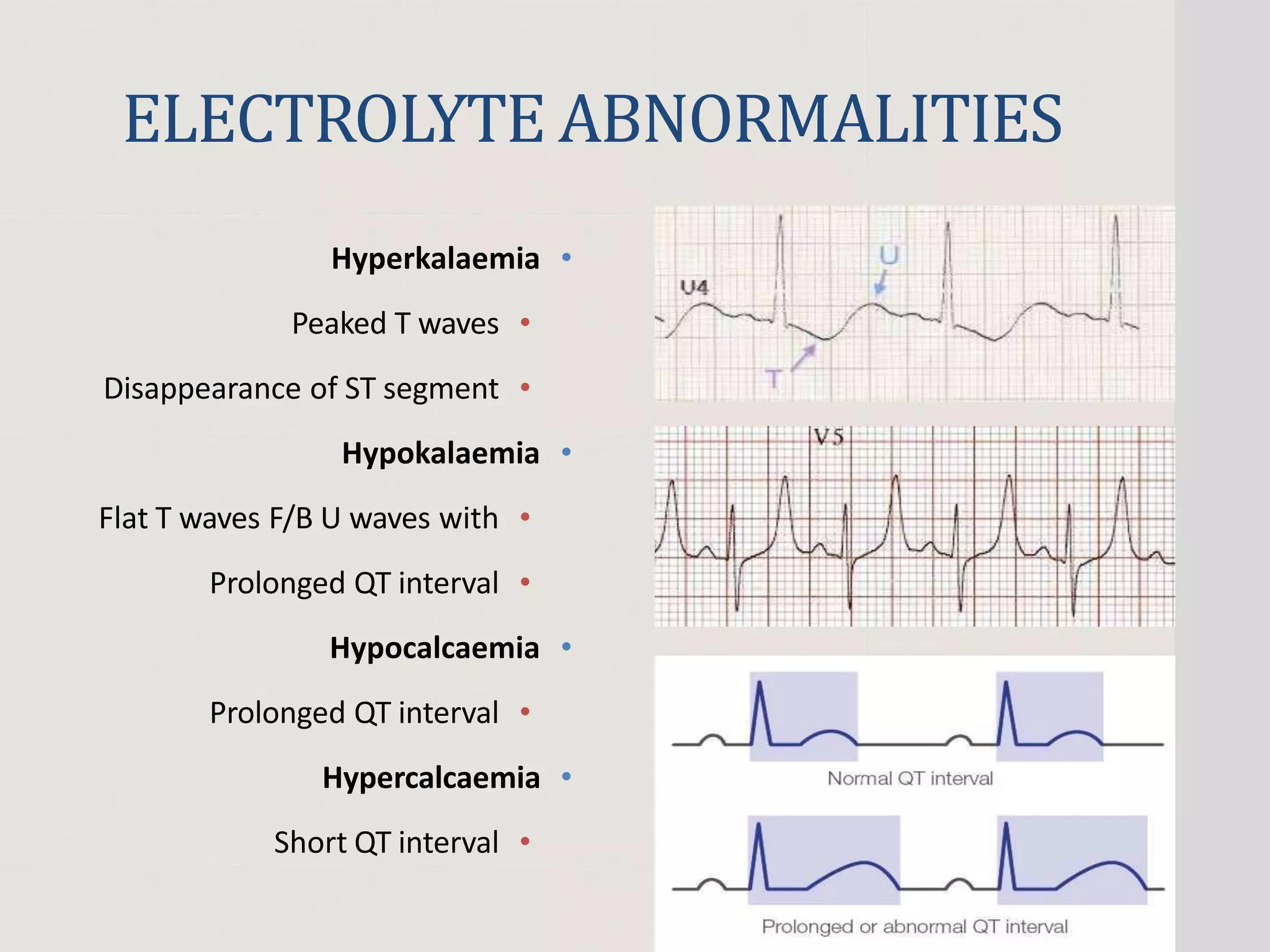
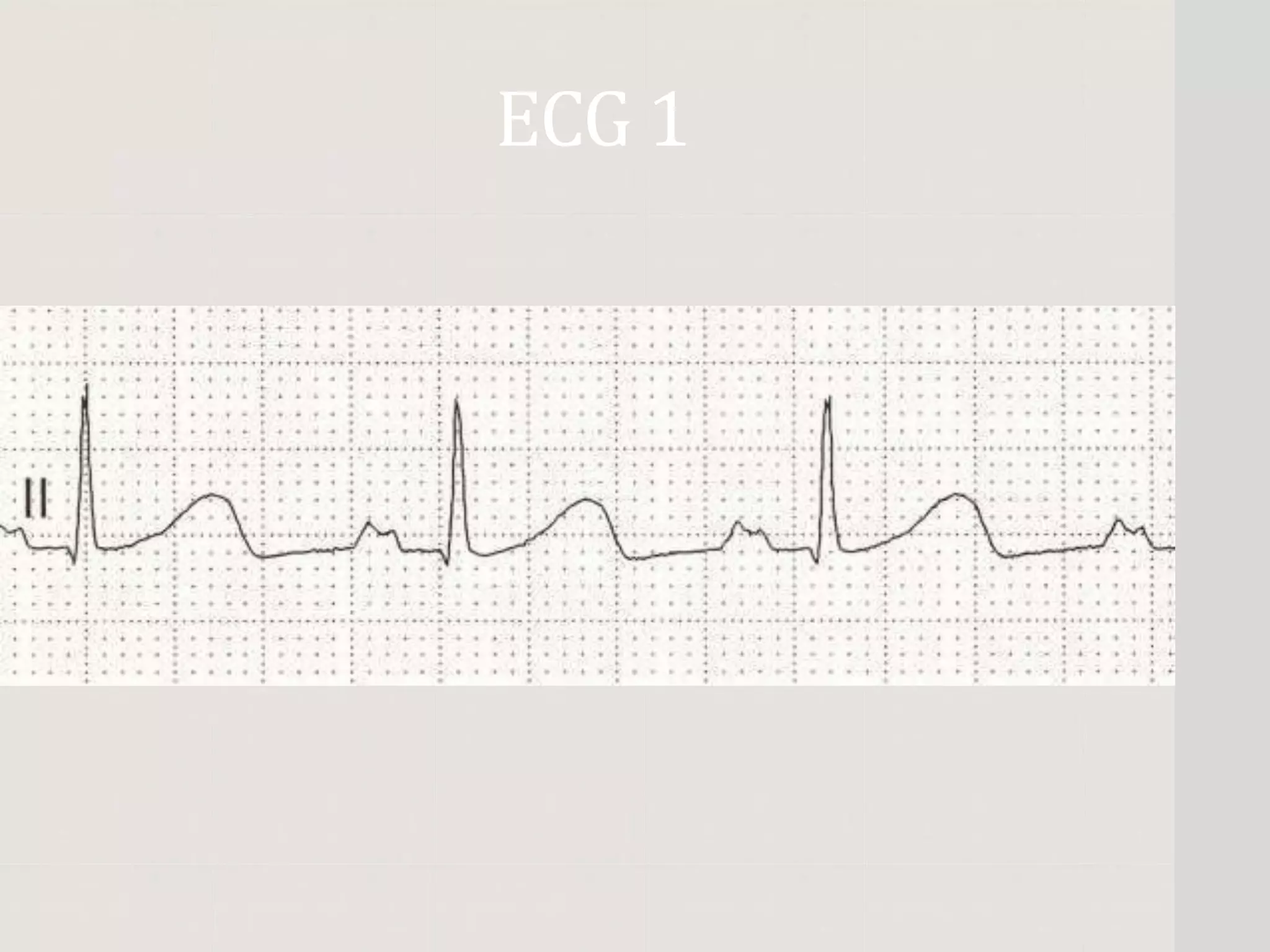
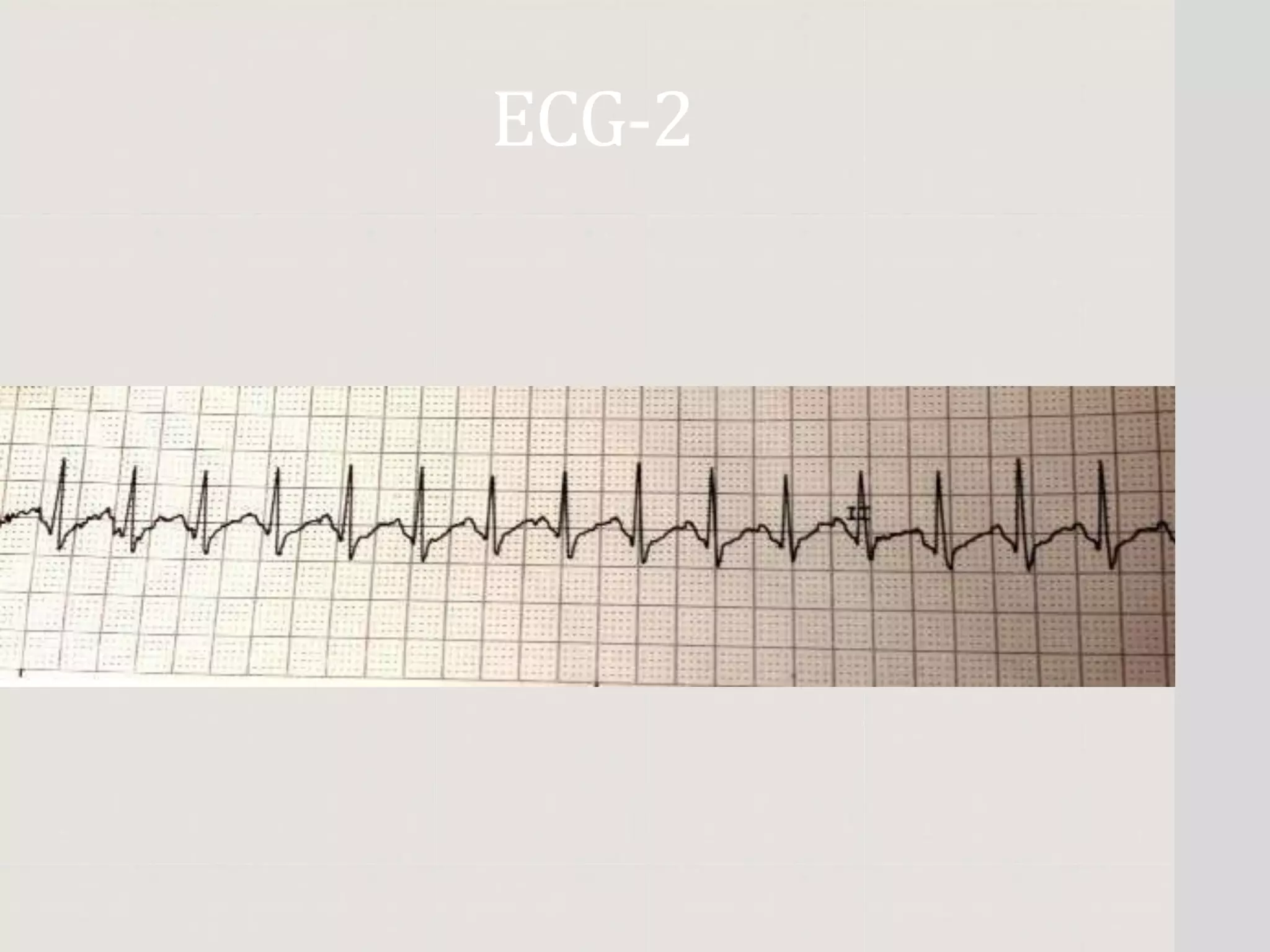
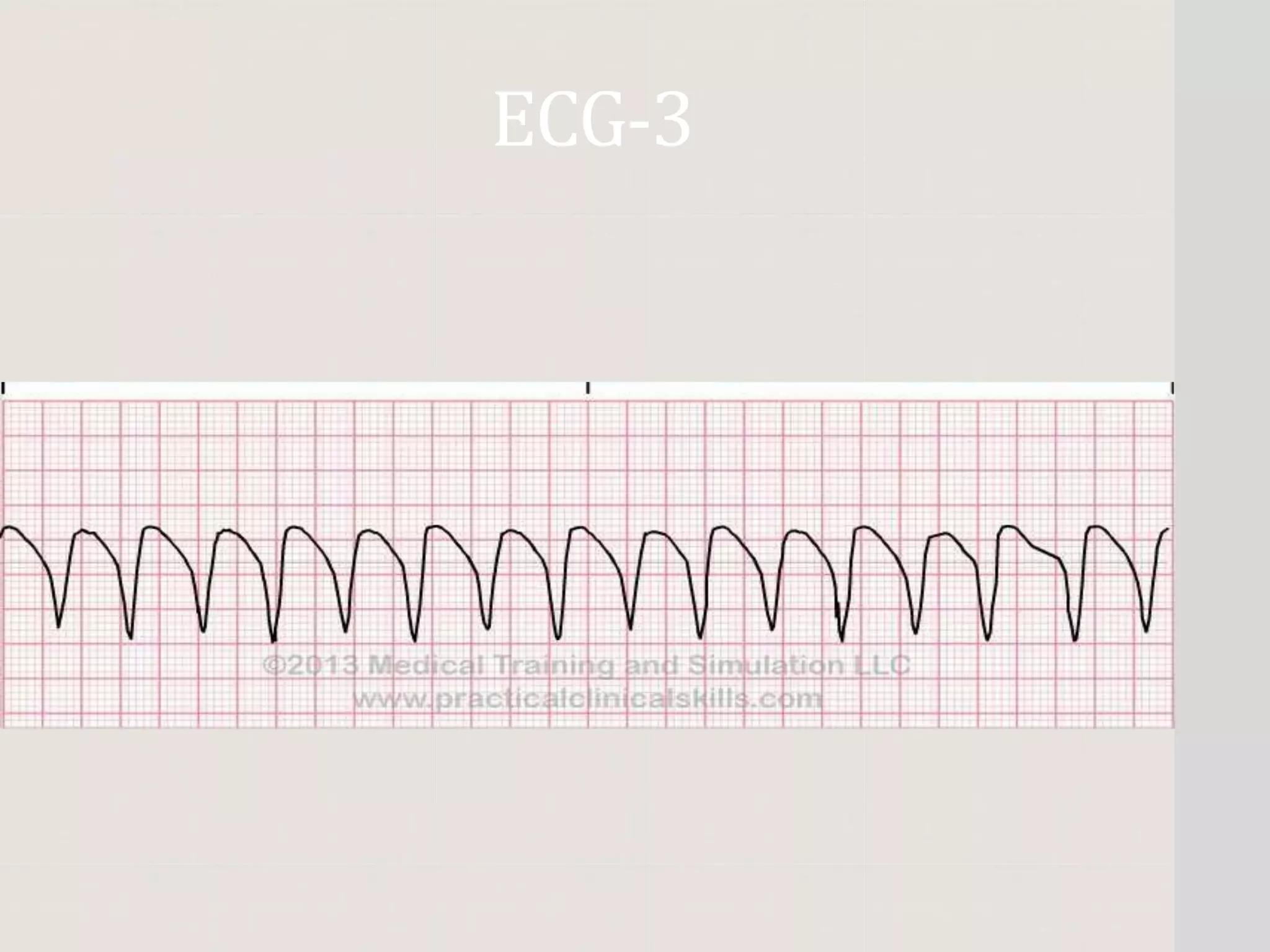
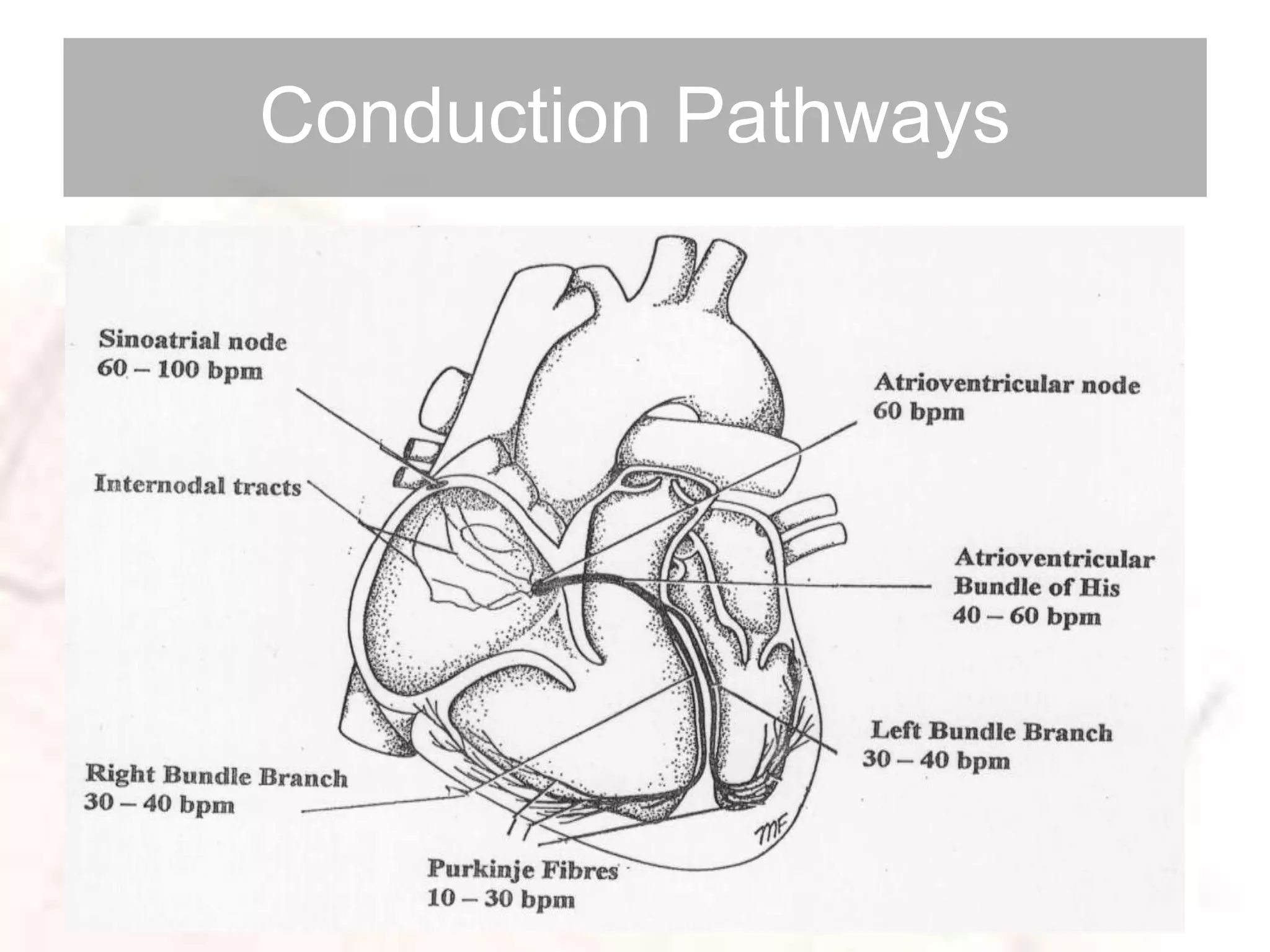
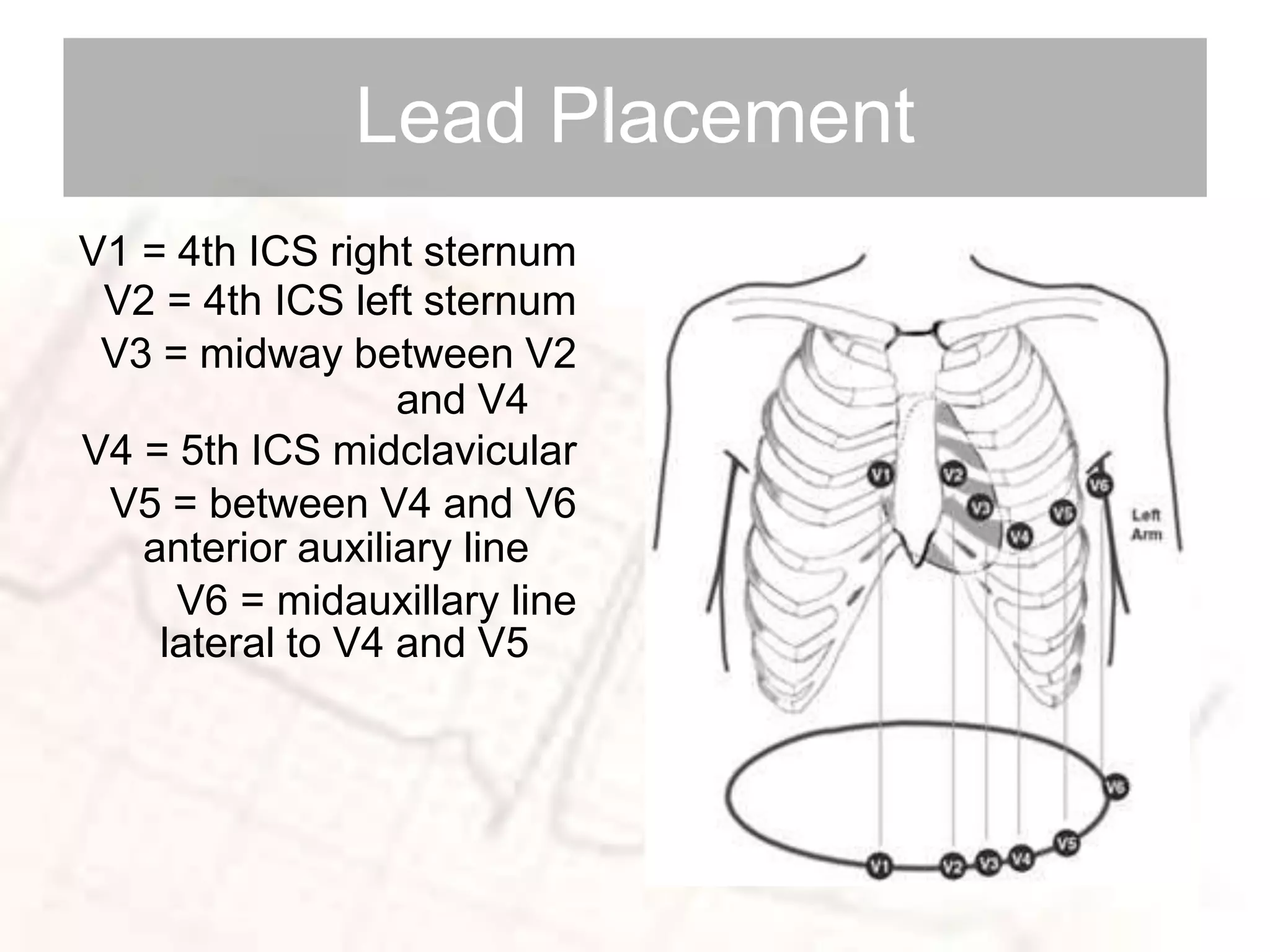
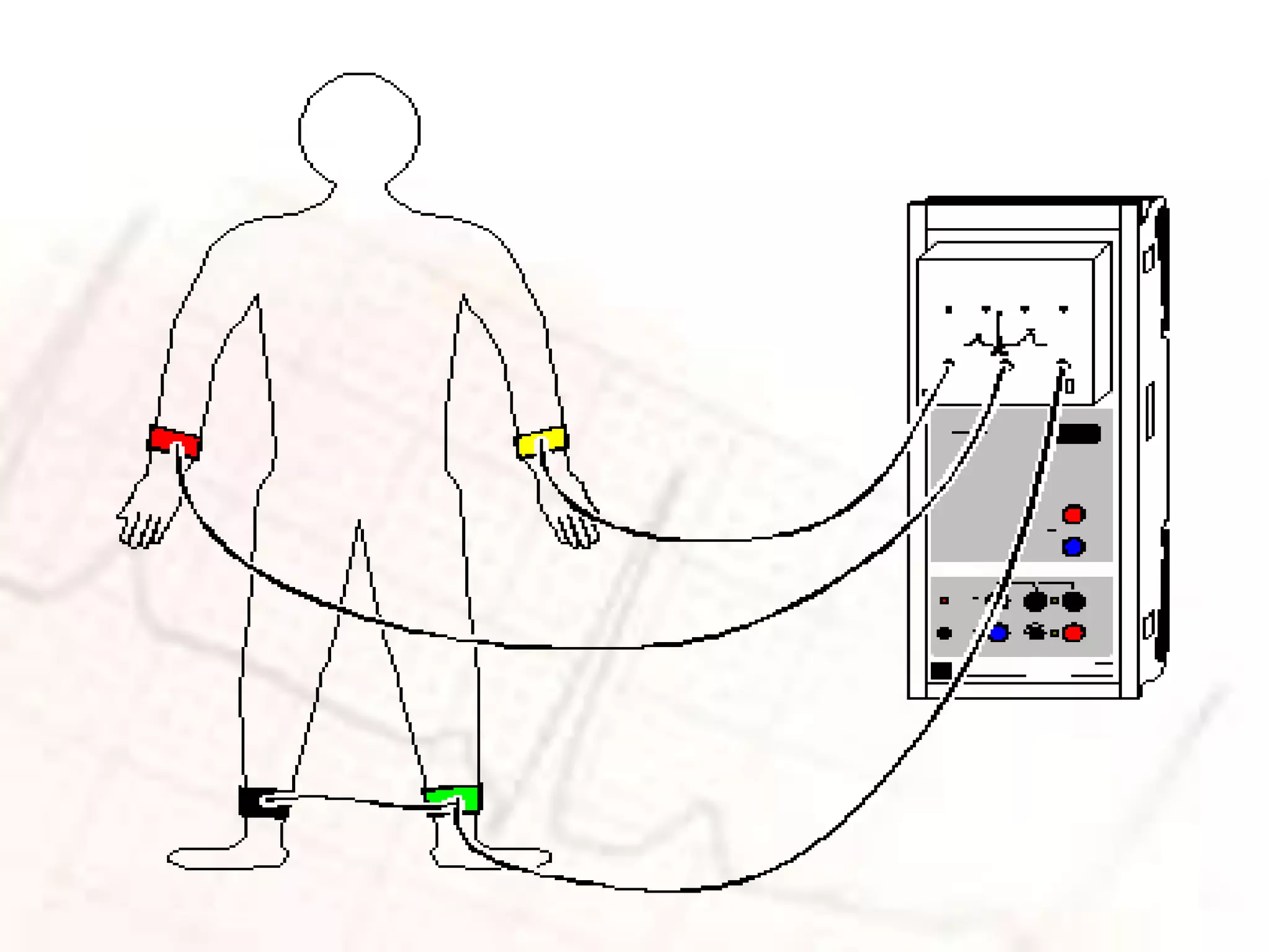
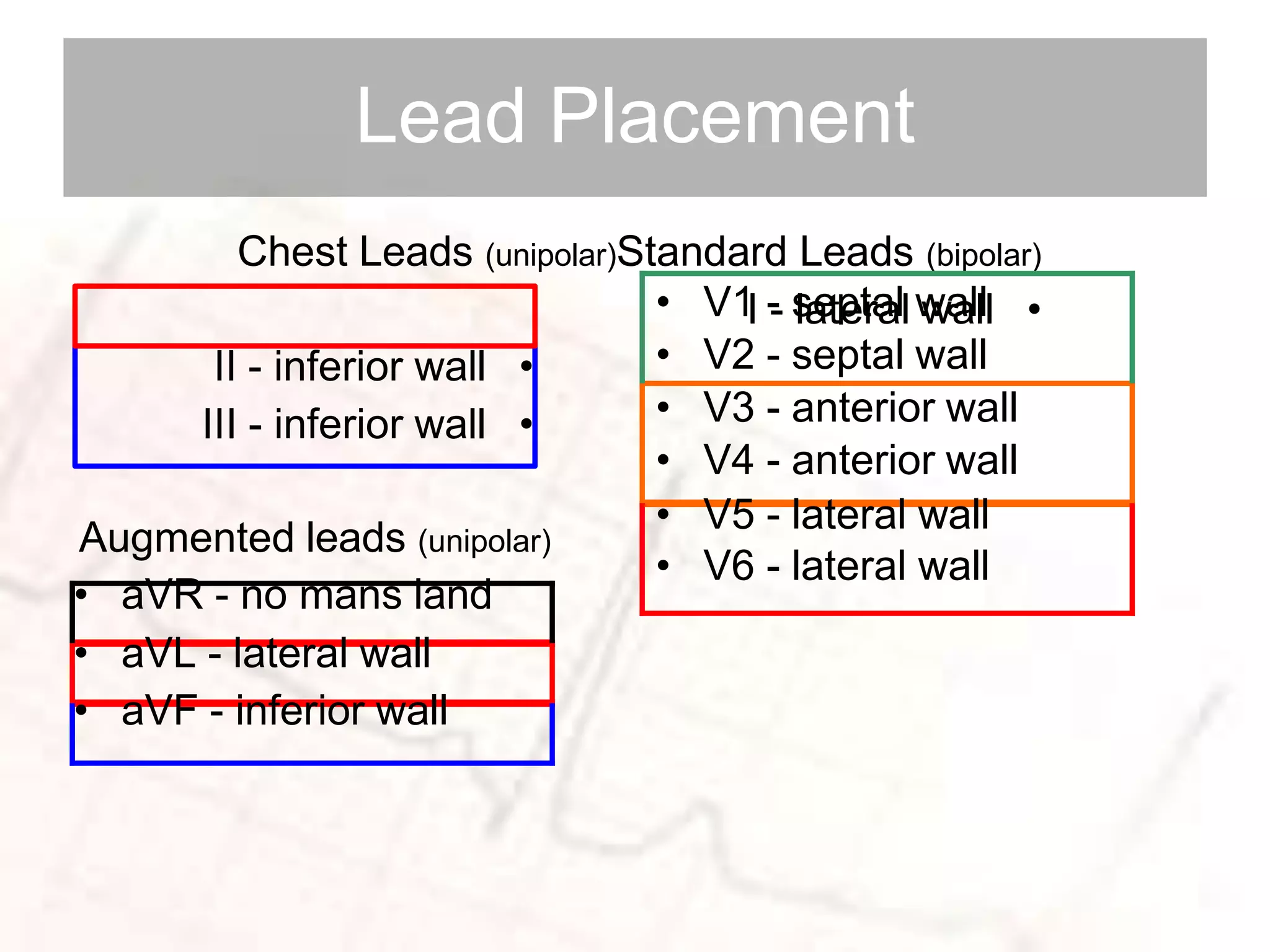
This document provides an overview of ECG interpretation, including conduction pathways, systematic interpretation techniques, and common abnormalities seen in critical care. It discusses lead placement and what different parts of the ECG represent. The document then covers various cardiac arrhythmias like sinus bradycardia, supraventricular tachycardia, atrial fibrillation, ventricular tachycardia, and heart block. It also discusses life-threatening arrhythmias, ST elevation myocardial infarction, and electrolyte abnormalities. Examples of different ECG tracings are presented to demonstrate various abnormalities.





![•
Rhythm = Regular or irregular. Map P-P and R-R
intervals
.
•
Rate = Number of P
’
s (atrial) R
’
s (ventricular)
per minute
)
6
second [
30
squares] X
10
=
(etar etunim
.
P rate:
8
x
10
=
80
R rate:
8
x
10
=
80
Interpretation](https://image.slidesharecdn.com/ecgechoplansunday-221010145326-03e383aa/75/basic-ECG-SAMPLE-WAY-12-2048.jpg)