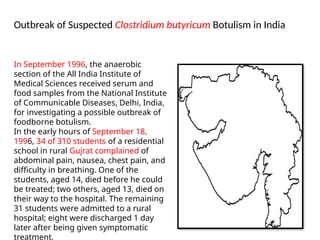
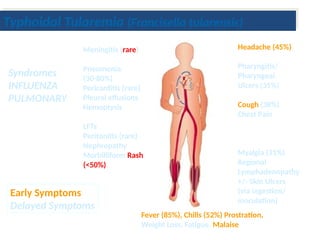
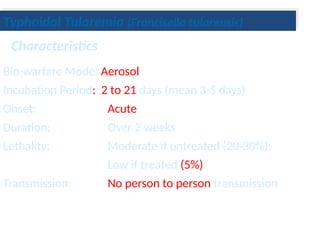
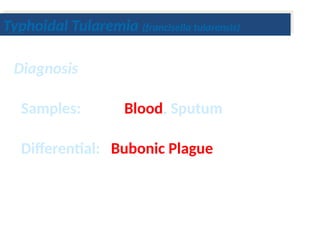
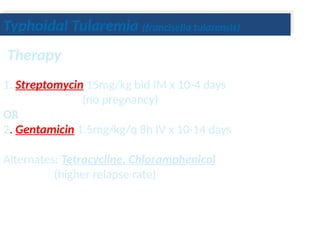
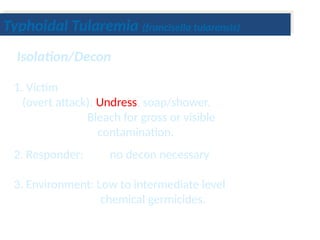
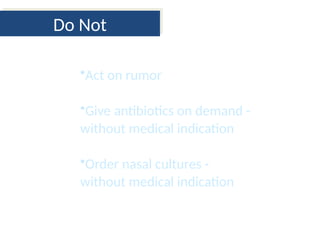
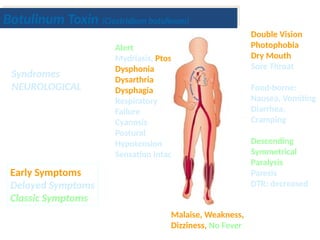
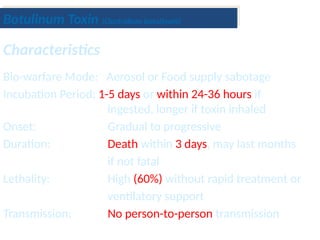
The document discusses biological terrorism syndromes, specifically detailing botulinum toxin and typhoidal tularemia, their symptoms, treatment, and historical outbreaks. It highlights the high lethality associated with botulinum toxin if untreated and the moderate risk of typhoidal tularemia, emphasizing the importance of rapid response and accurate diagnosis. Additionally, it provides recommendations for isolation, decontamination, and prevention measures for both syndromes.
![TIMELINE
1820-Justinus Kerner, a small-town German medical officer and
romantic poet, gave the first complete description of clinical botulism
based on extensive clinical observations of so-called “sausage
poisoning
1875- Émile van Ermengem, professor of bacteriology and a student of
Robert Koch, correctly described Clostridium botulinum as the bacterial
source of the toxin.
World War II-weaponization of botulinum toxin was investigated at Fort
Detrick in Maryland. Carl Lamanna and James Duff[40]
developed the
concentration and crystallization techniques that Edward J. Schantz
used to create the first clinical product.](https://image.slidesharecdn.com/barath-240814052552-7a9dfda2/85/barath-pptx-zoonotic-pathogens-and-control-4-320.jpg)