The document discusses postpartum adaptations and provides information on:
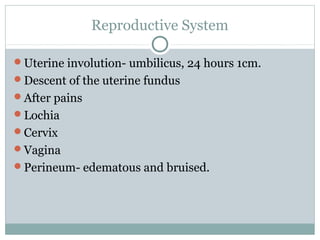
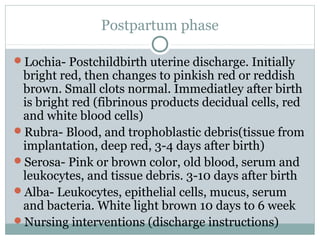
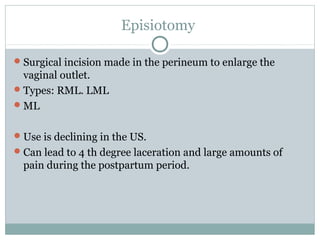
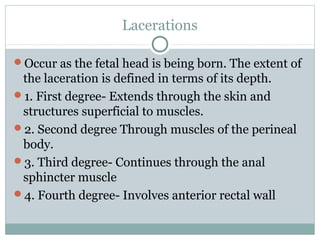
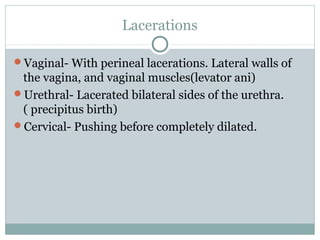
1. Common postpartum changes such as uterine involution, lochia, perineal changes, and cardiovascular, urinary, and lactation adaptations.
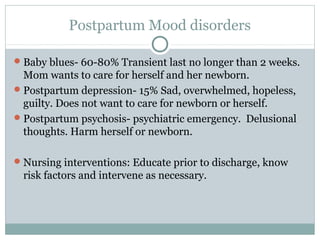
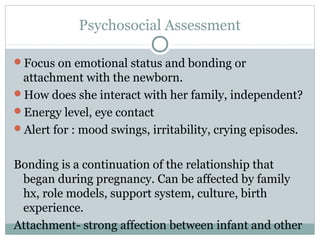
2. Cultural influences and psychosocial factors like attachment, maternal role development, and postpartum mood disorders.
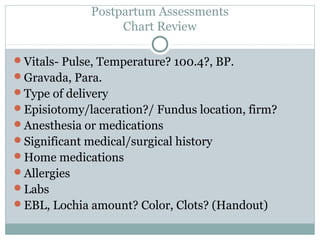
3. Nursing assessments and priorities for postpartum care including physical assessments, teaching self-care, and monitoring for complications like hemorrhage and infection.