The document discusses the flaws in a safety program developed solely by upper management, emphasizing the importance of employee involvement for its success. Recommendations include dismantling the current program and reconstructing it through a committee of at least 50% employees to better address safety concerns across various departments. It also touches on the issue of workplace behavior and the need for proactive management in dealing with employees' personal issues affecting safety.



![delivery of nursing and healthcare services.
15
Sample Content
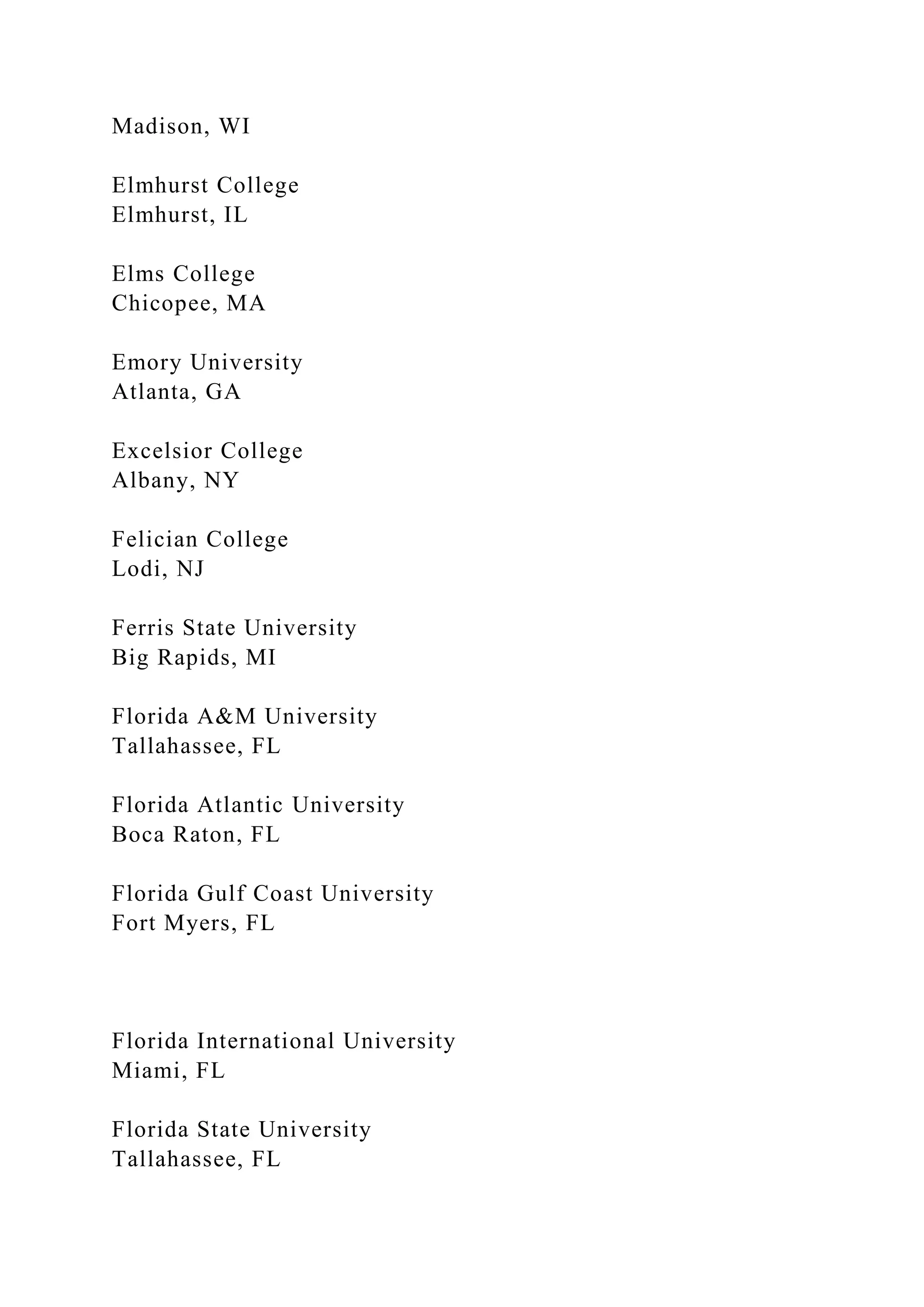
• Quality improvement models differentiating structure, process,
and outcome indicators
• Principles of a just culture and relationship to analyzing errors
• Quality improvement methods and tools: Brainstorming,
Fishbone cause and effect
diagram, flow chart, Plan, Do Study, Act (PDSA), Plan, Do,
Check, Act (PDCA),Find,
Organize, Clarify, Understand, Select-Plan, Do, Check, Act
(FOCUS-PDCA), Six Sigma,
Lean
• High-Reliability Organizations (HROs) / High-reliability
techniques
• National patient safety goals and other relevant regulatory
standards (e.g., CMS core
measures, pay for performance indicators, and never events)
• Nurse-sensitive indicators
• Data management (e.g., collection tools, display techniques,
data analysis, trend
analysis, control charts)
•Analysis of errors (e.g., Root Cause Analysis [RCA], Failure
Mode Effects Analysis
[FMEA], serious safety events)
• Communication (e.g., hands-off communication, chain-of-
command, error disclosure)
• Participate in executive patient safety rounds
• Simulation training in a variety of settings (e.g., disasters,
codes, and other high-risk](https://image.slidesharecdn.com/bh1-230107175604-a8918d31/75/B-H1-The-first-issue-that-jumped-out-to-me-is-that-the-presiden-docx-57-2048.jpg)


![Institute of Medicine. (2003). Health professions education: A
bridge to quality.
Washington, DC: National Academies Press.
Institute of Medicine. (2004). Keeping patients safe:
Transforming the work environment
of nurses. Washington, DC: National Academies Press.
Institute of Medicine. (2005). Building a better delivery system:
A new
engineering/health care partnership. Washington, DC: National
Academies Press.
Institute of Medicine. (2008). Retooling for an aging America:
Building the healthcare
workforce. Washington, DC: National Academies Press.
Institute of Medicine. (2009). Redesigning continuing education
in the health
professions. Washington, DC: National Academies Press.
Institute of Medicine. (2010). Robert Wood Johnson Foundation
initiative on the future
of nursing, at the Institute of Medicine. Retrieved on February
16, 2010, from
http://www.iom.edu/Activities/Workforce/Nursing.aspx
Interprofessional Professionalism Collaborative. (2008).
Interprofessional
professionalism: What’s all the fuss? [PowerPoint slides].
Presented at the
American Physical Therapy Meeting on February 7, 2008, in
Nashville, TN.](https://image.slidesharecdn.com/bh1-230107175604-a8918d31/75/B-H1-The-first-issue-that-jumped-out-to-me-is-that-the-presiden-docx-118-2048.jpg)
![National Institutes of Health. (2009). Family history and
improving health [PDF
document]. Retrieved from panel statement:
http://consensus.nih.gov/2009/familyhistorystatement.htm
46
National Priorities Partnership. (2008). National priorities and
goals: Aligning our efforts
to transform america’s healthcare. Washington, DC: National
Quality Forum.
National Research Council. (2005). Advancing the nation’s
health needs: NIH research
training programs. Washington. DC: National Academies Press.
Nelson, E., Batalden, P., & Godfrey, M. (2007). Quality by
design: a clinical
microsystems approach. San Francisco: Jossey Bass.
Nelson, E. C., Godfrey, M. M., Batalden, P. B., Berry, S. A.,
Bothe, A. E., McKinley,
K.E. et al. (2008). Clinical microsystems, Part 1. The building
blocks of health
systems. The Joint Commission Journal on Quality and Patient
Safety, 34(7),
367-378.
O’Connell, M. B., Korner, E. J., Rickles, N. M., & Sias, J. J.
(2007). Cultural competence
in health care and its implications for pharmacy Part 1](https://image.slidesharecdn.com/bh1-230107175604-a8918d31/75/B-H1-The-first-issue-that-jumped-out-to-me-is-that-the-presiden-docx-121-2048.jpg)