The document provides a comprehensive overview of intestinal obstruction, detailing its types, clinical features, and diagnostic approaches including imaging techniques like CT and ultrasound. It discusses the causes of both small bowel and large bowel obstructions, highlighting intrinsic and extrinsic factors, as well as differentiating simple from complicated obstructions. Additionally, it emphasizes the importance of identifying the transition point and includes various imaging findings associated with specific causes, like Crohn's disease, neoplasia, and adhesions.







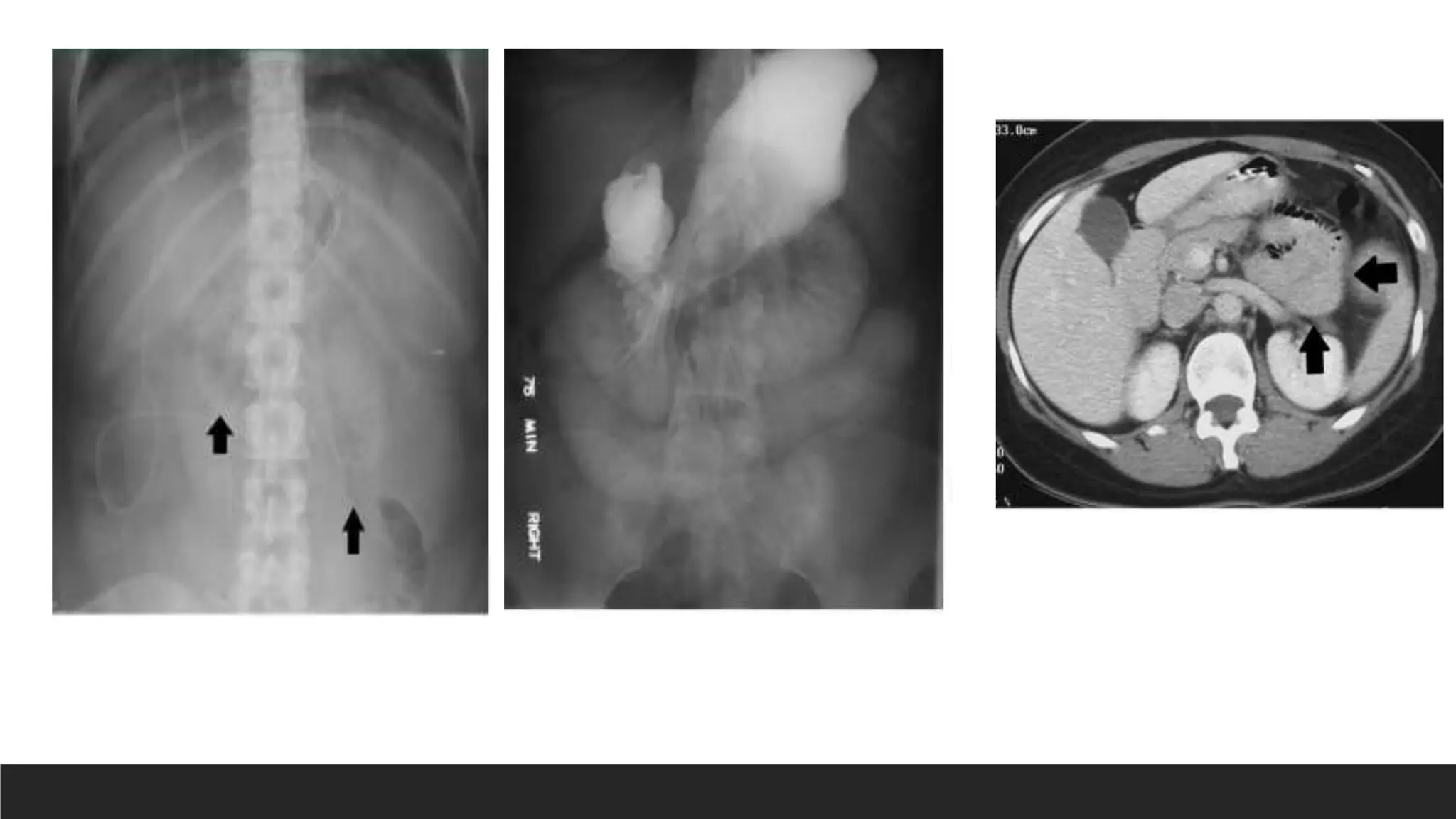

















































![Colorectal carcinoma
Common sites-sigmoid colon and splenic flexure.
The most common site of perforation[3%–8%] in LBO is not at the site of the tumor but
at the cecum
Barium enema
seen as filling defects
appear as exophytic or sessile masses
may be circumferential -apple core sign
CT
Asymmetric and short-segment colonic wall thickening
or an enhancing soft-tissue mass centered in the colon that narrows the colonic lumen
Pericolonic lymph nodes](https://image.slidesharecdn.com/approachtointestinalobstruction-240503145117-07bbd539/75/Approach-to-intestinal-obstructions-pptx-58-2048.jpg)





















