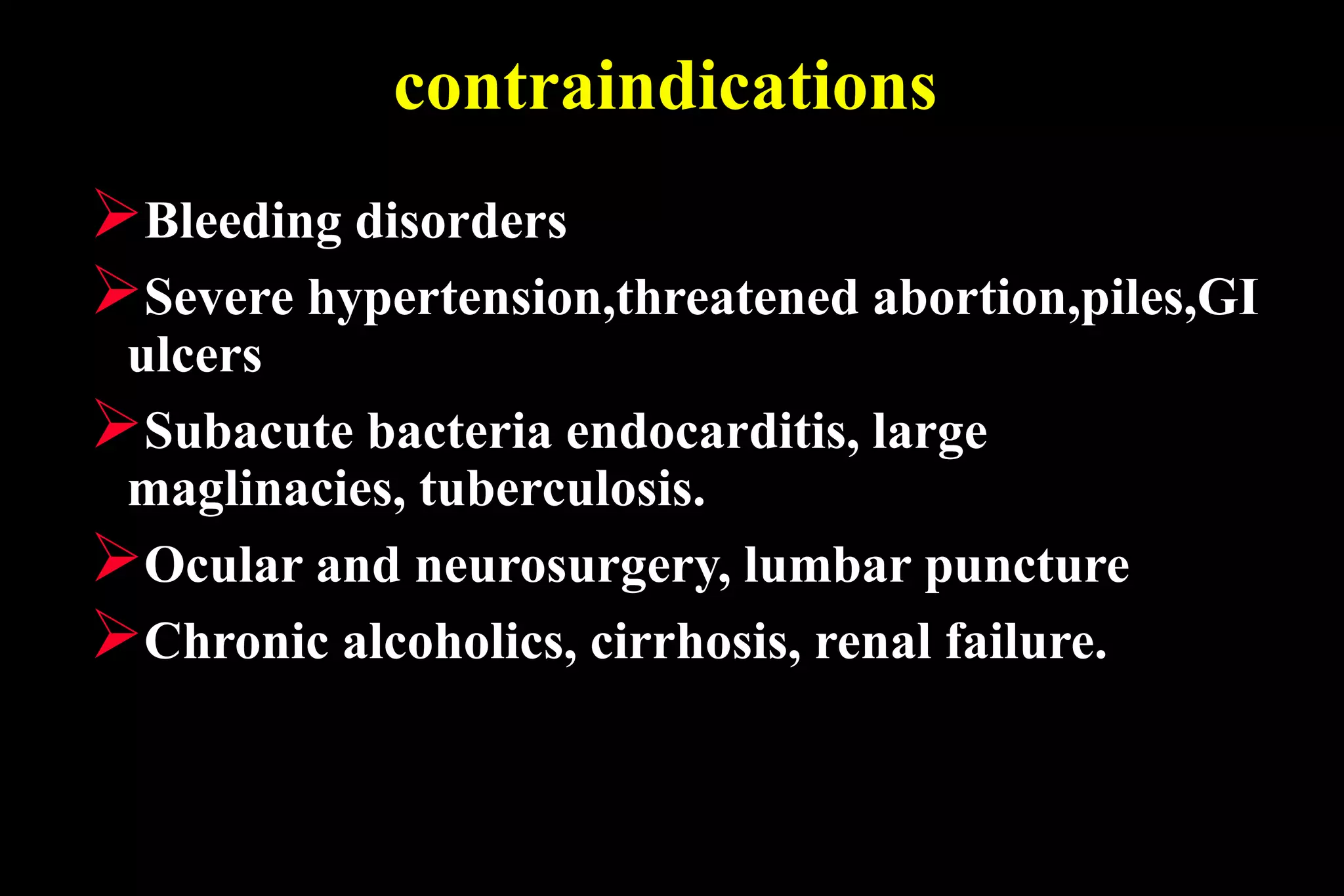
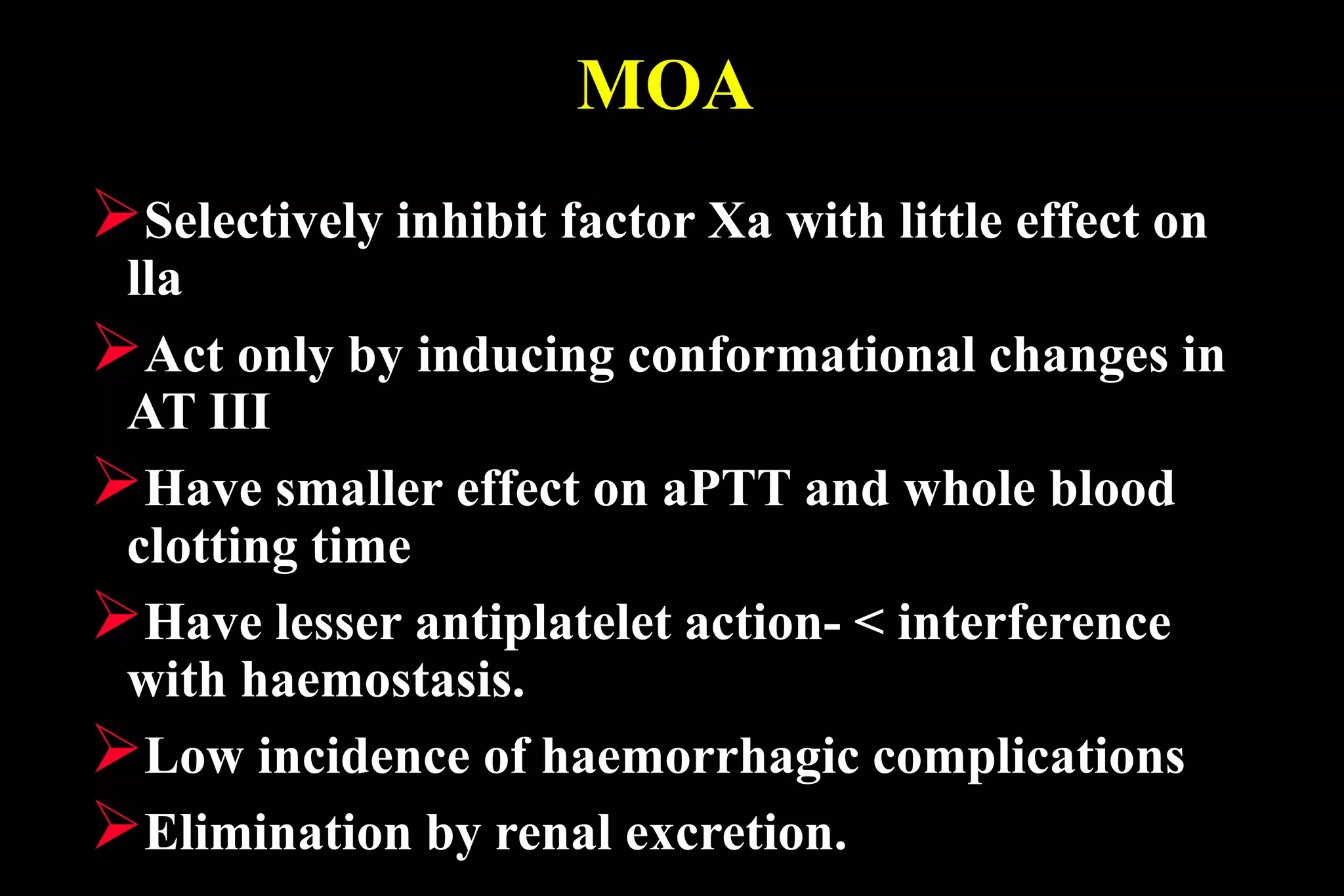
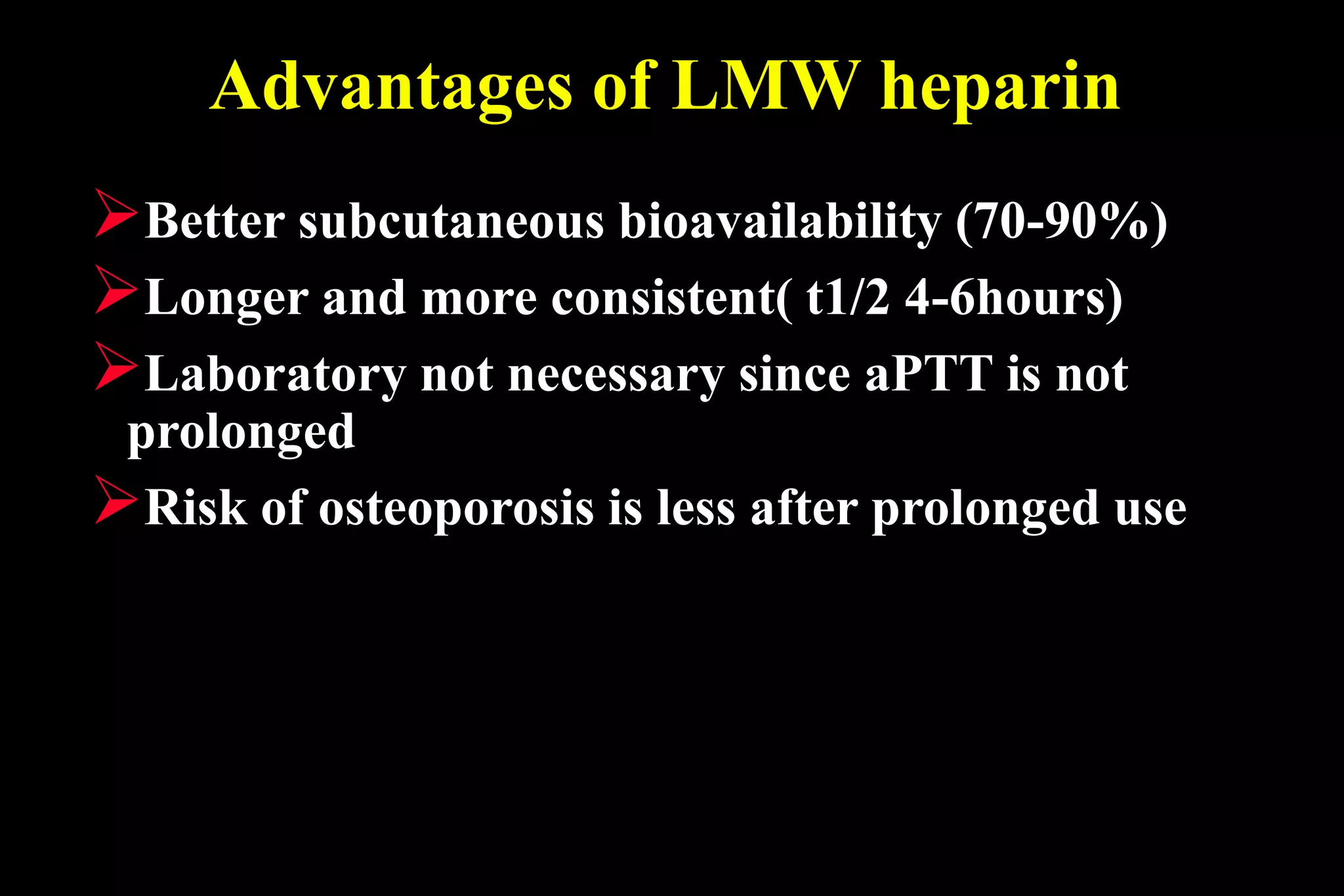
This document discusses anticoagulant and antiplatelet drugs. It describes heparin, low molecular weight heparins like enoxaparin, and warfarin as common anticoagulants. Heparin prevents clotting by activating antithrombin III which inactivates clotting factors. Warfarin inhibits vitamin K dependent clotting factors. Antiplatelet drugs discussed include aspirin, dipyridamole, ticlopidine, and clopidogrel. Aspirin inhibits thromboxane A2 while clopidogrel and ticlopidine block ADP receptors on platelets. These drugs are used to prevent thromboembolic disorders and complications from