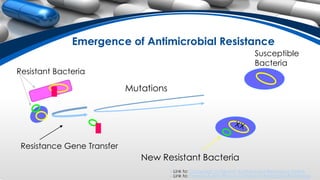
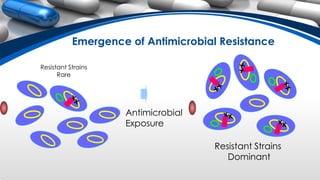
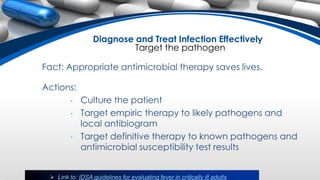
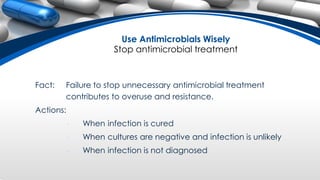
Antibiotic resistance occurs when bacteria evolve and become resistant to antibiotics through overuse and misuse of antibiotics. When antibiotics are prescribed unnecessarily or not taken as directed, it can allow bacteria to survive and spread antibiotic resistance. To prevent further antibiotic resistance, antibiotics should only be taken as prescribed by a doctor, all of the prescribed antibiotics should be taken, and leftover antibiotics should not be used or shared with others.