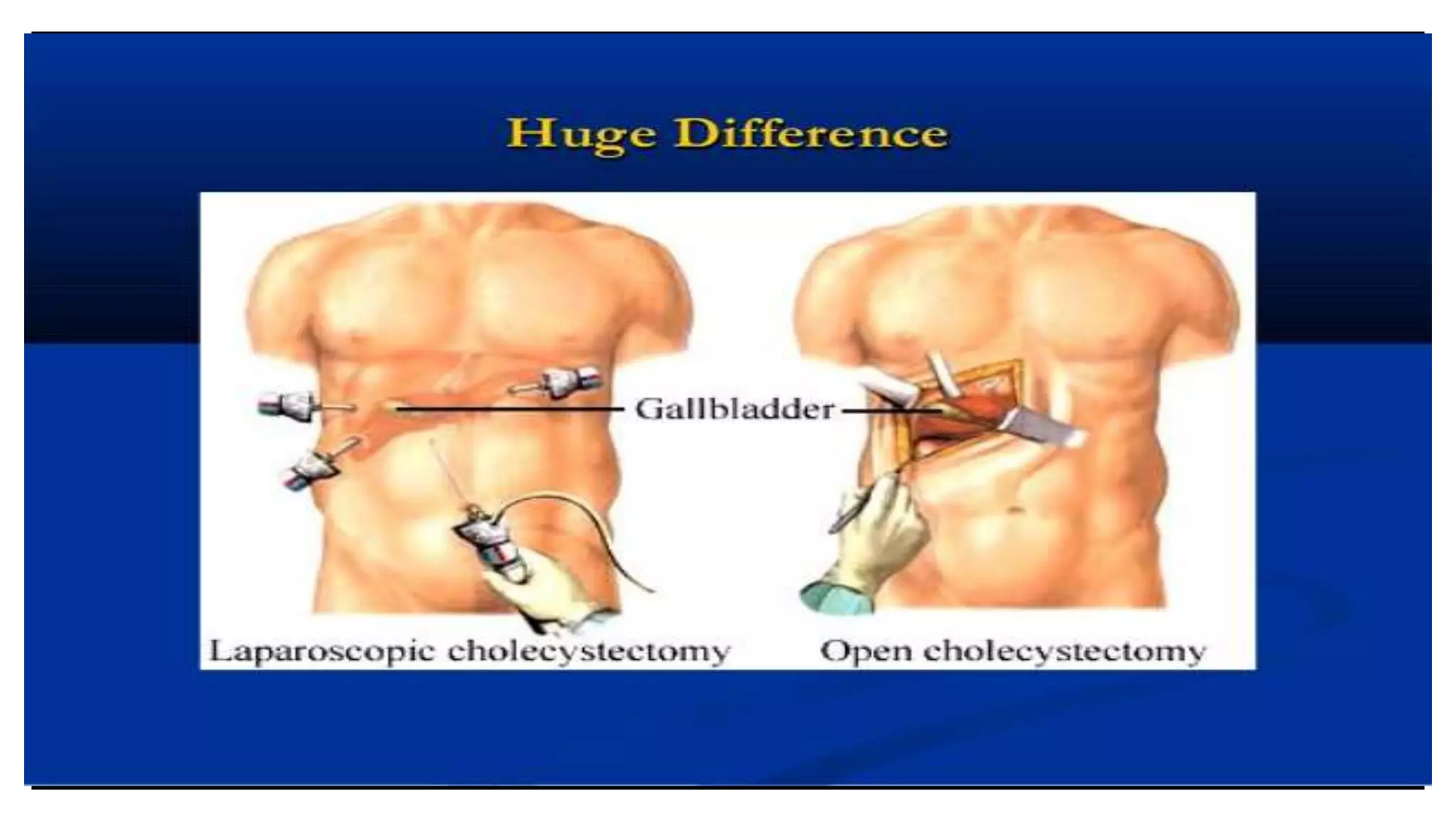
This document discusses the anesthesia considerations for laparoscopic surgery, covering indications, advantages, disadvantages, contraindications, and anesthetic techniques. It highlights various factors affecting anesthesia management, such as positioning, gas insufflation, and the effects of pneumoperitoneum on multiple bodily systems. The document concludes with insights on preoperative, intraoperative, and postoperative management to optimize patient outcomes.