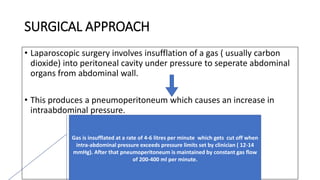
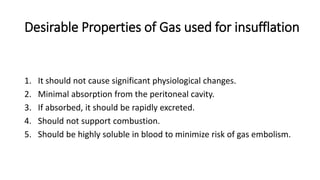
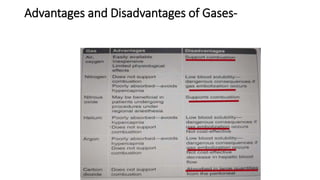
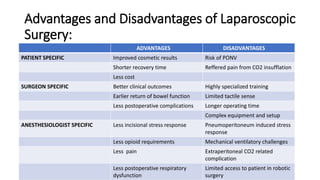
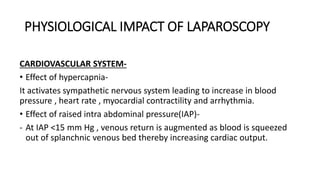
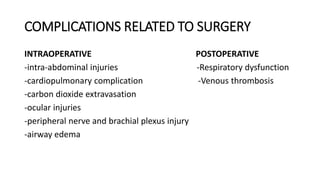
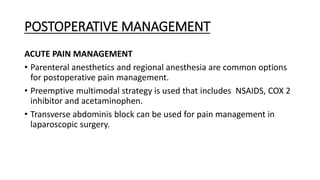
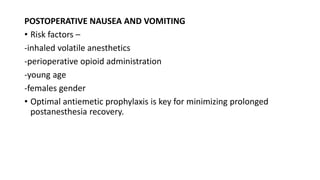
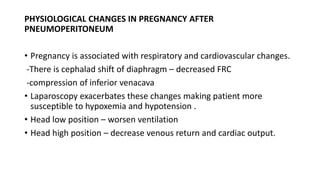
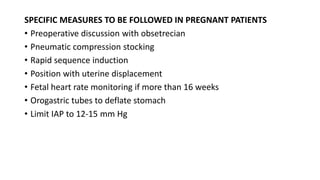
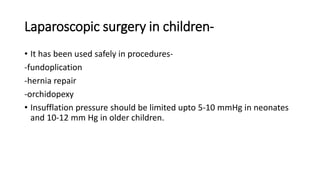
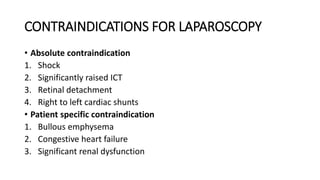
Laparoscopic surgery involves inserting specialized tubes into the abdominal cavity to perform minimally invasive surgery. Carbon dioxide gas is used to insufflate the abdomen and create pneumoperitoneum. This causes physiological changes including increased heart rate and blood pressure due to hypercapnia and raised intra-abdominal pressure. It can also decrease lung volumes and compliance. The anesthesiologist must carefully manage ventilation and monitor for potential complications like subcutaneous emphysema, capnothorax, and venous gas embolism during laparoscopic surgery. Patient positioning, temperature control, and multimodal postoperative pain management are also important considerations for the anesthesiologist.

![shalini laparo [Autosaved].pptx](https://image.slidesharecdn.com/shalinilaproautosaved-231107054900-e5005f6e/85/shalini-laparo-Autosaved-pptx-34-320.jpg)