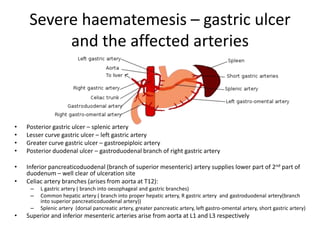
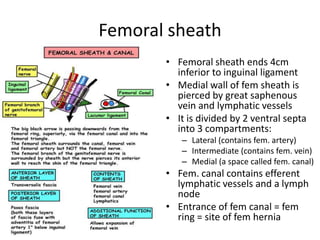
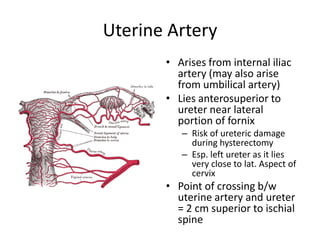
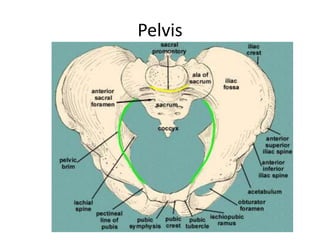
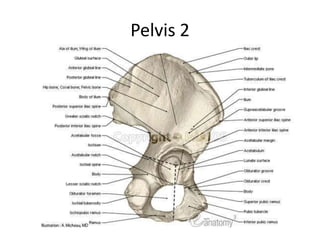
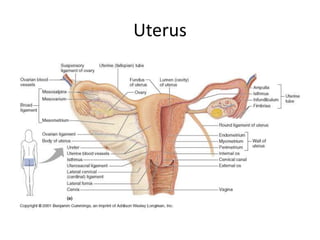
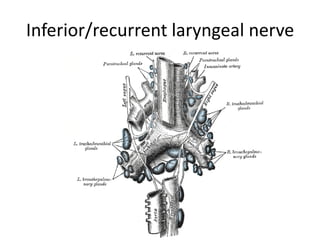
This document summarizes various anatomical structures and their blood supply. It discusses the arteries associated with gastric ulcers in different locations. It also reviews the blood supply to the liver, the course of the psoas major muscle, structures within the femoral sheath, the origin of the uterine artery, and pelvic anatomy. Key nerves like the hypoglossal and recurrent laryngeal nerves are also outlined.