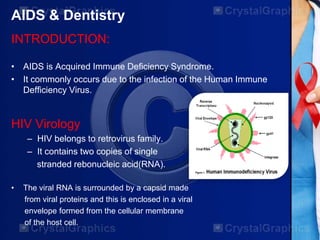
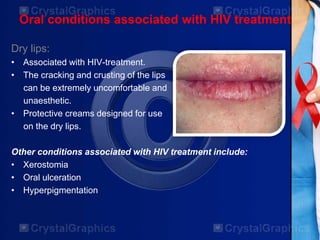
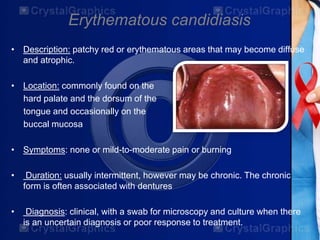
The document discusses the relationship between HIV/AIDS and dentistry, including the virology, transmission, and various oral conditions associated with HIV infection. It highlights the importance of infection control, ethical considerations, and presents a study exploring HIV stage as a risk factor for periodontal status in HIV-positive patients. The findings suggest that smoking and oral hygiene habits significantly influence periodontal health, rather than HIV stage or age.