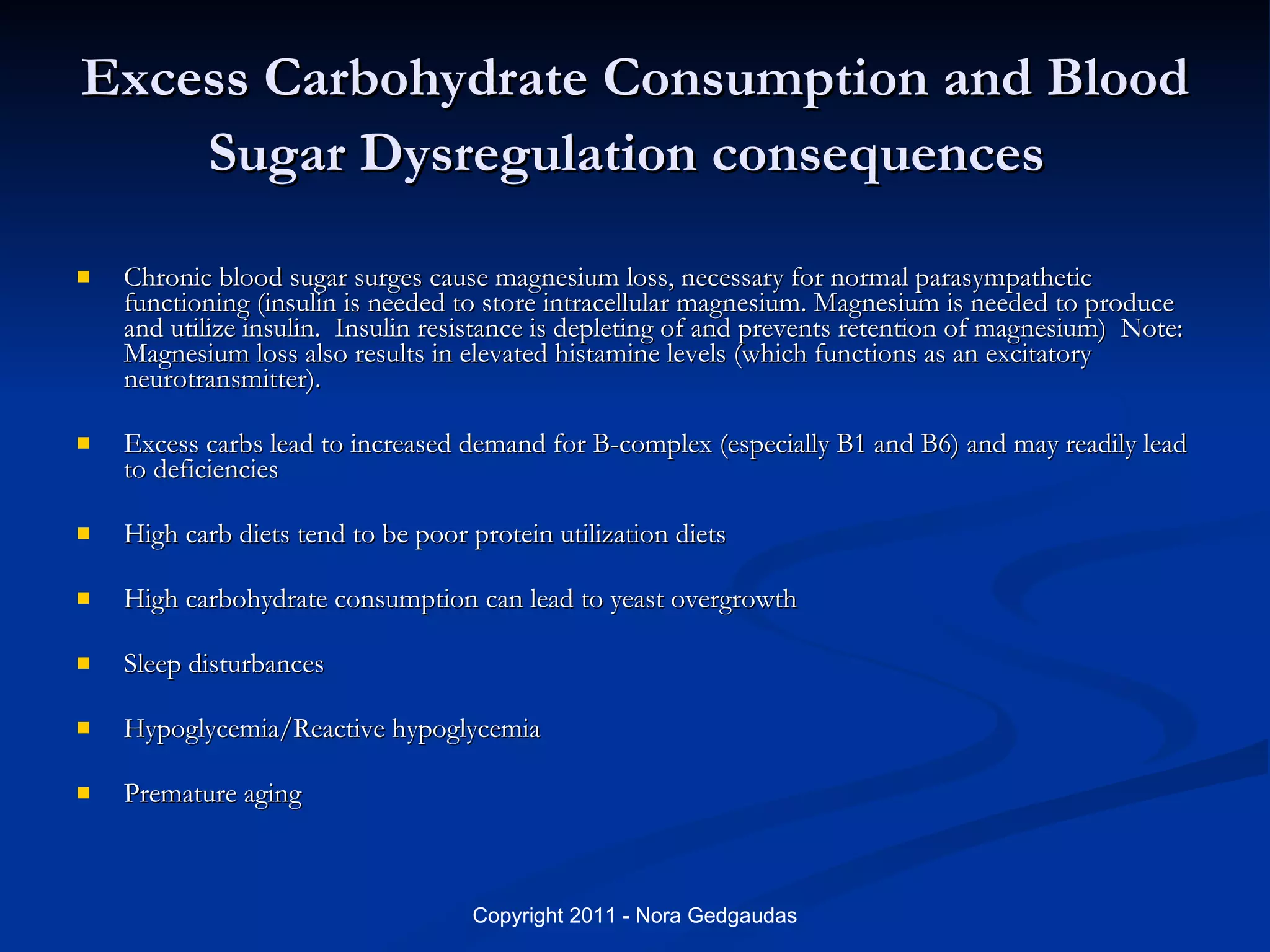
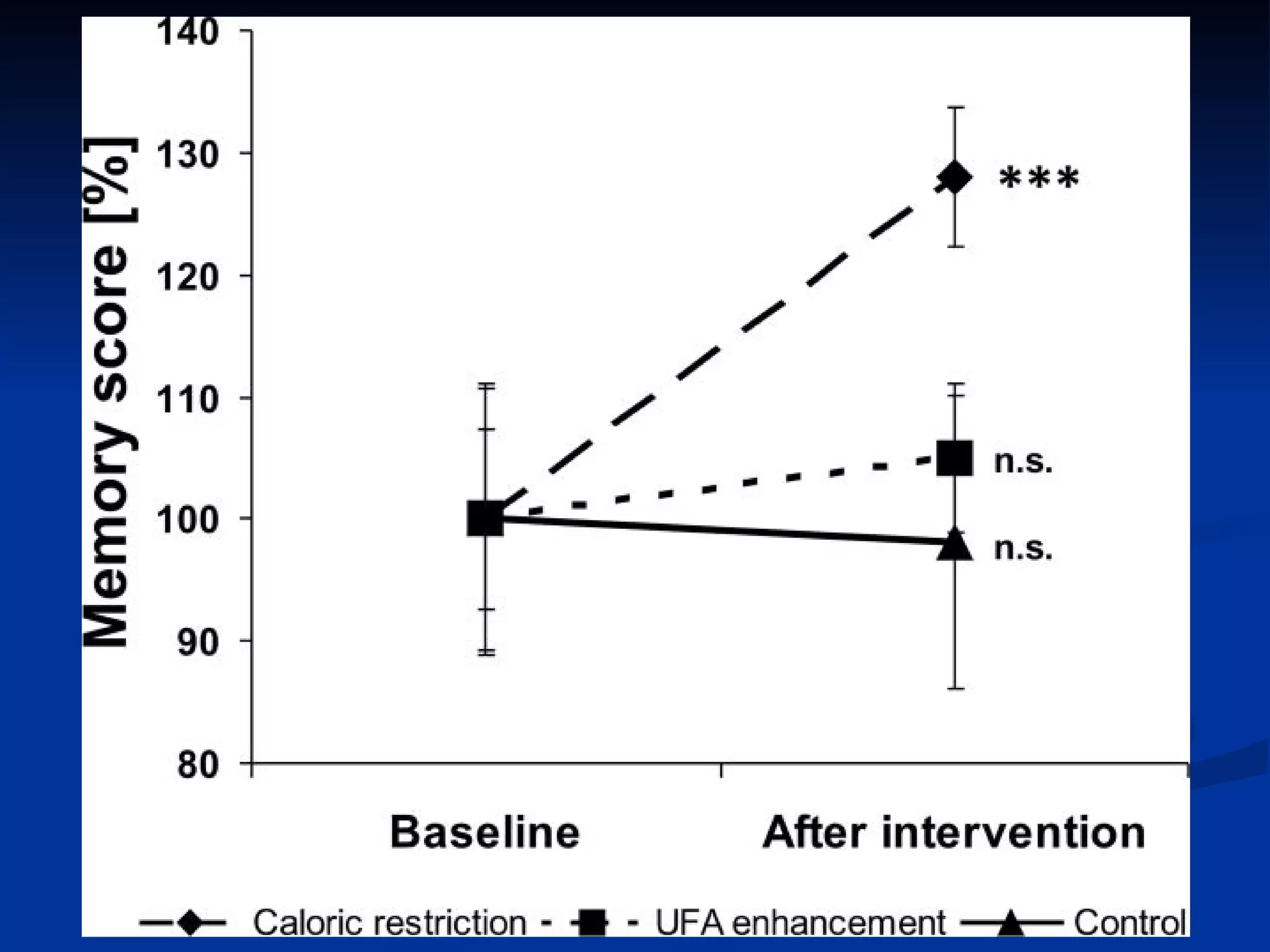
The document discusses how nutrition and diet are closely linked to mental health and functioning. Chronic high carbohydrate consumption and blood sugar imbalances can negatively impact the brain and nervous system over time, potentially leading to issues like anxiety, depression, cognitive decline, and Alzheimer's disease. Addressing underlying nutritional deficiencies, food sensitivities, and blood sugar regulation is seen as essential for optimal mental wellness and stability.