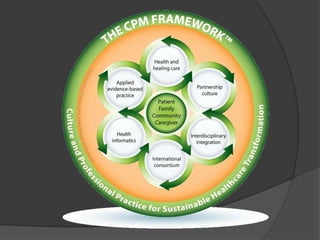
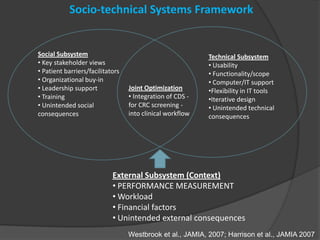
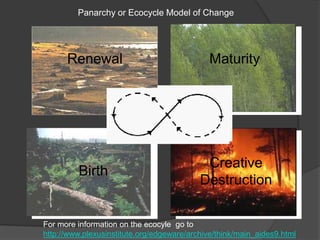
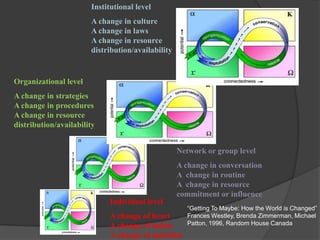
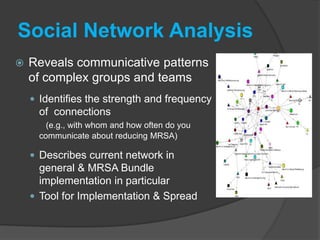
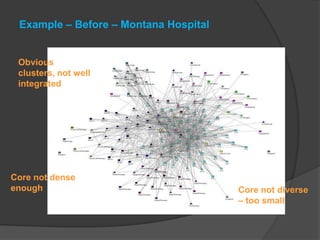
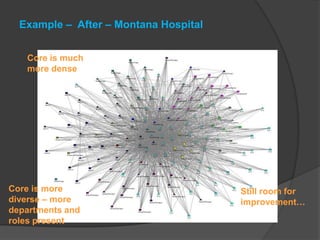
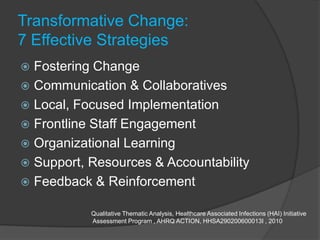
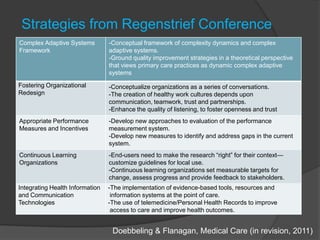
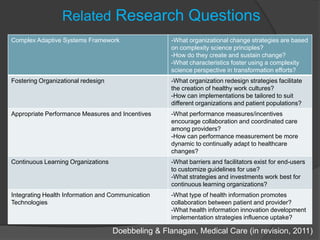
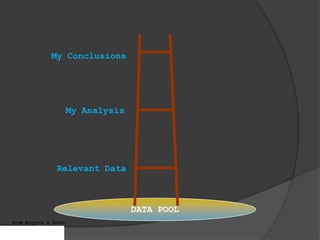
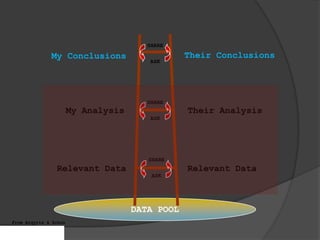
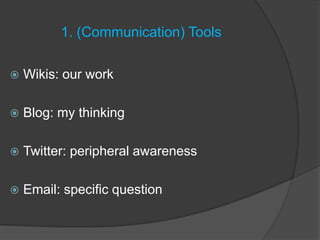
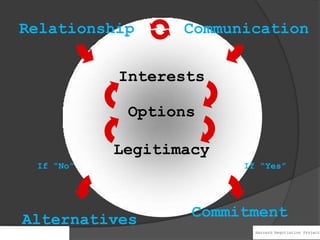
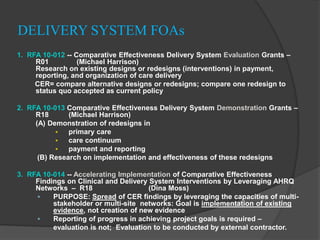
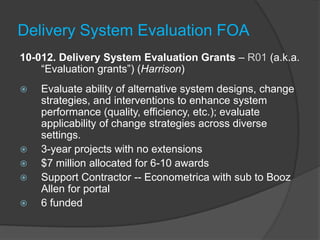
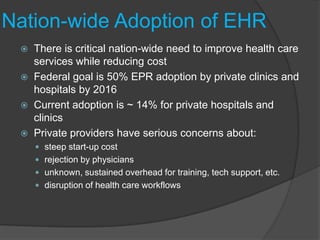
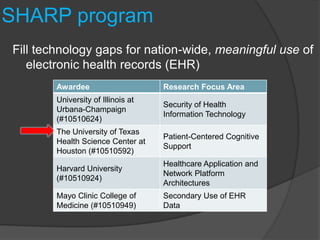
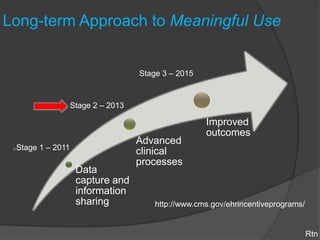
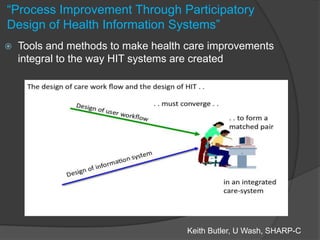
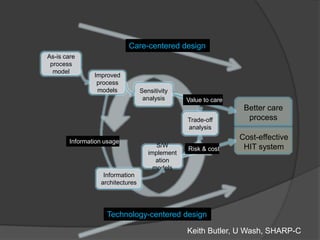
The document discusses strategies for transforming healthcare through evidence-based practices, partnerships, and technology, presented at the 19th International Conference in San Francisco. Key themes include fostering organizational change, the importance of communication and collaboration, and integrating health information technologies to improve patient outcomes. It emphasizes a complex adaptive systems approach and continuous learning to enhance healthcare quality and efficiency.