This document provides an overview of acute pancreatitis including:
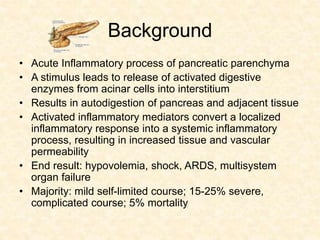
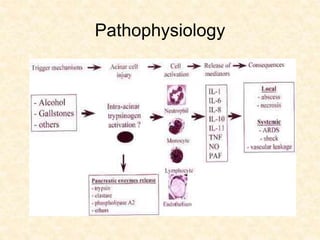
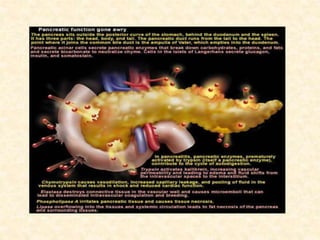
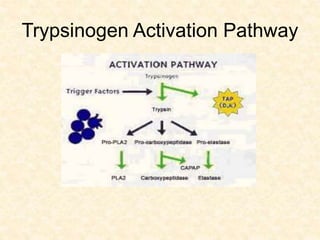
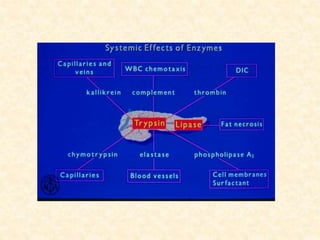
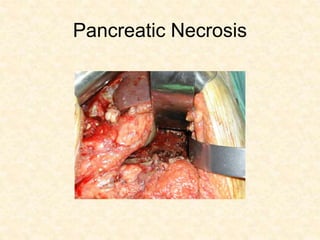
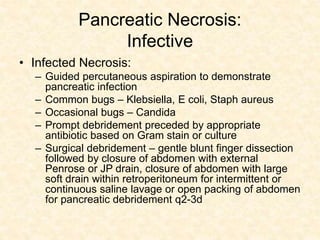
- The pathophysiology of premature activation of digestive enzymes within the pancreas leading to autodigestion.
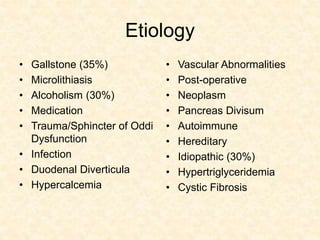
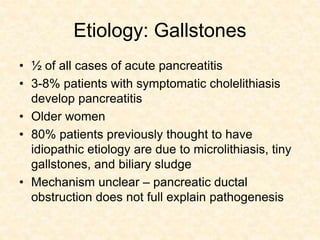
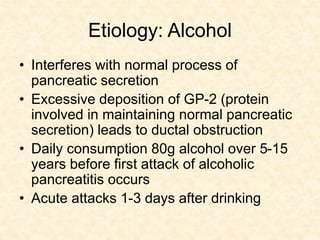
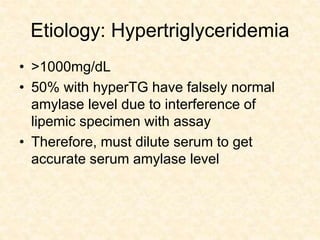
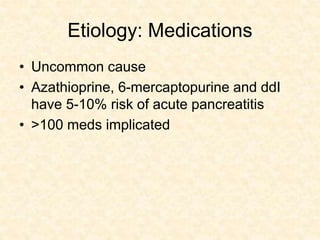
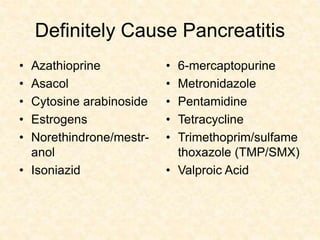
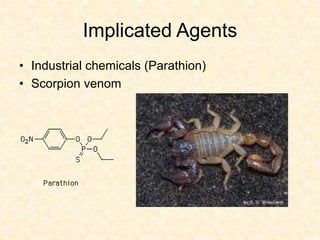
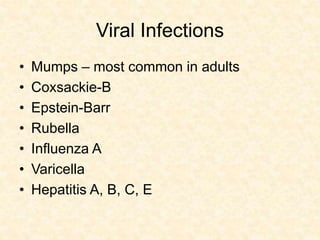
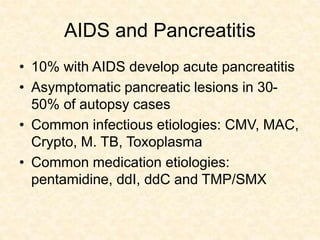
- Common etiologies like gallstones, alcohol use, and hypertriglyceridemia.
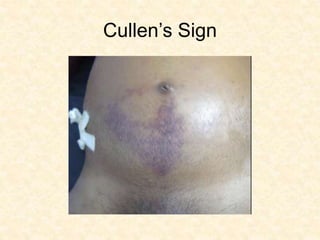
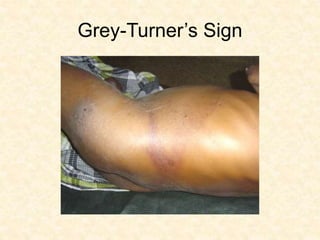
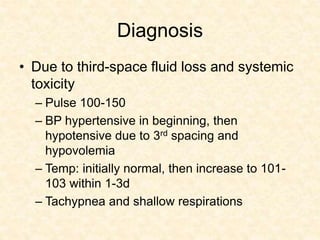
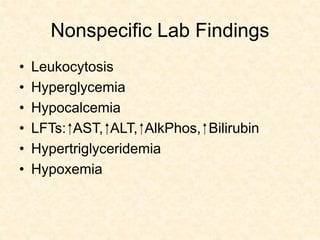
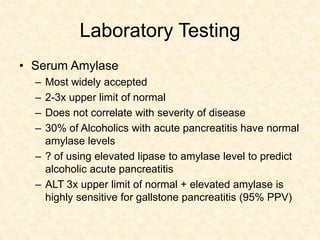
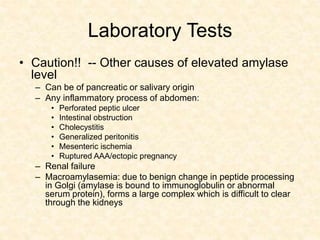
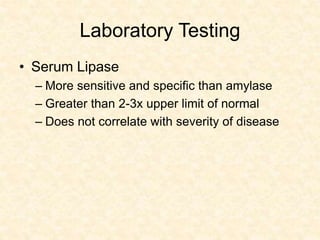
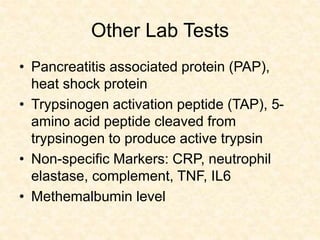
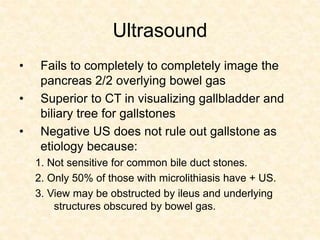
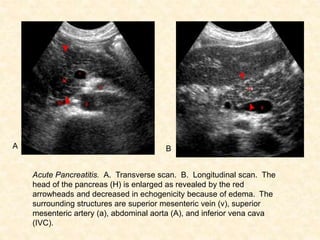
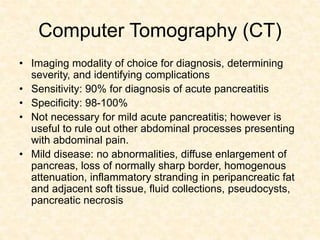
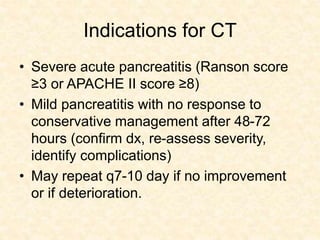
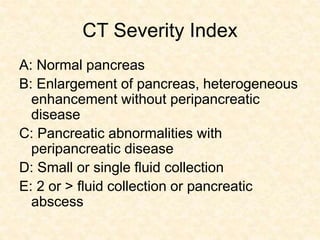
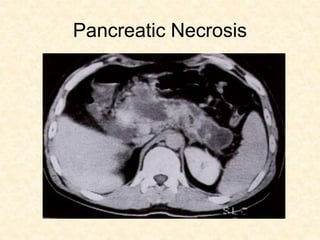
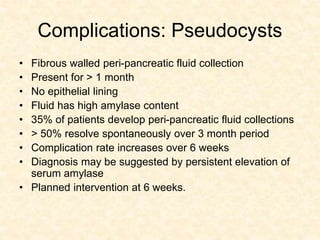
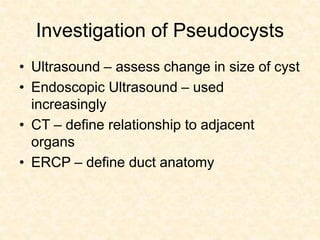
- Diagnosis through clinical signs/symptoms confirmed with lab tests like serum amylase and lipase levels or imaging like CT.
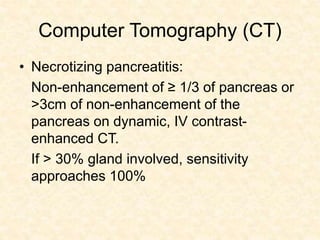
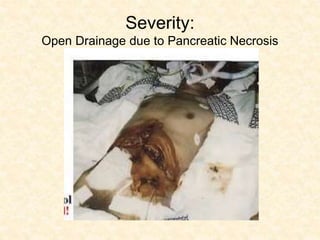
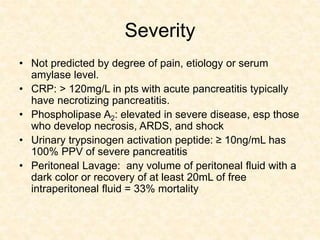
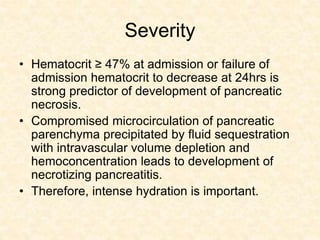
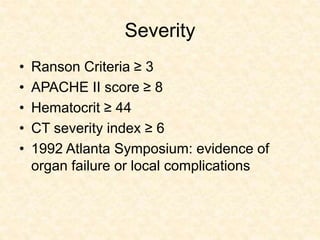
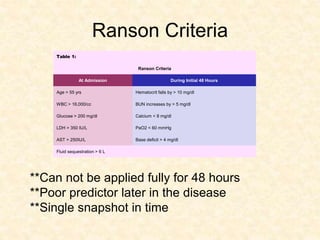
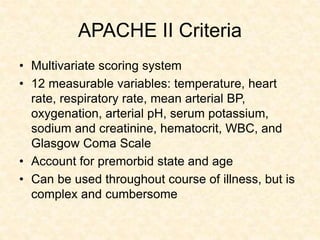
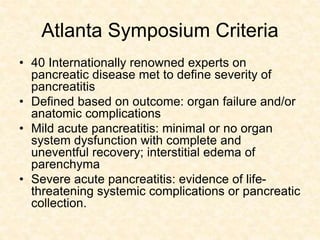
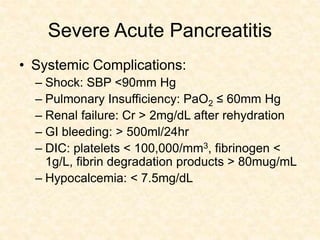
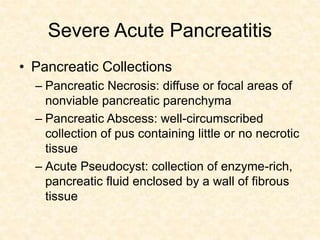
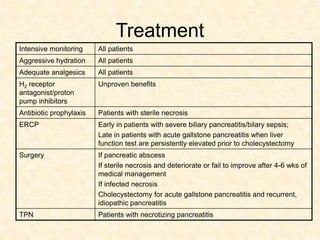
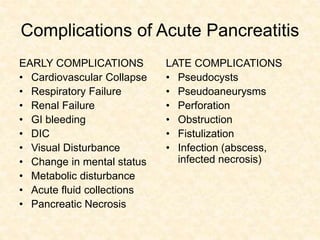
- Determining severity using criteria like Ranson score, APACHE II score, or evidence of organ failure/necrosis on CT.
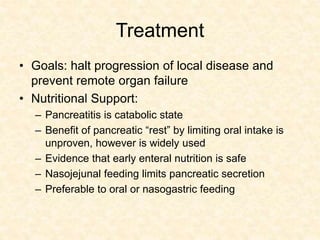
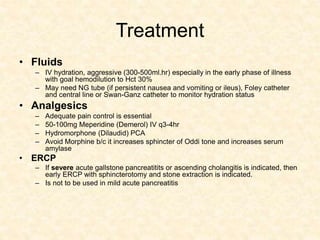
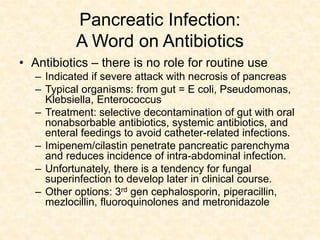
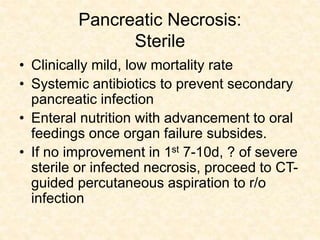
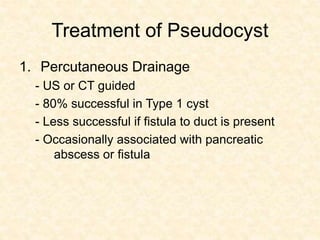
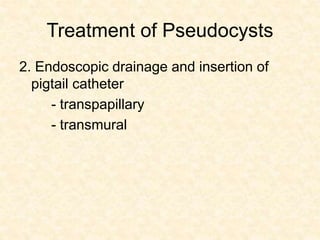
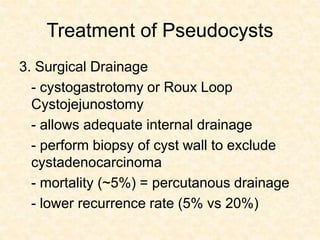
- Goals of treatment include halting disease progression, preventing organ failure through aggressive hydration and nutritional support, adequate pain control, and ERCP for severe gall