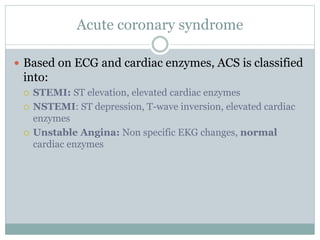
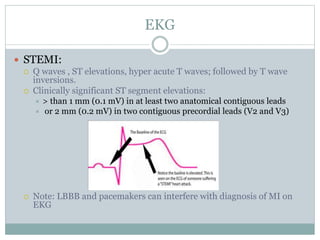
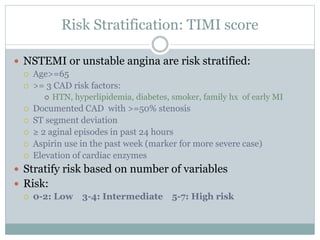
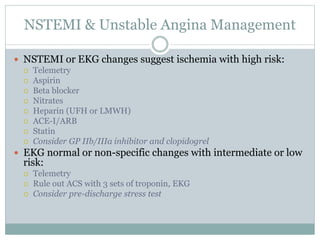
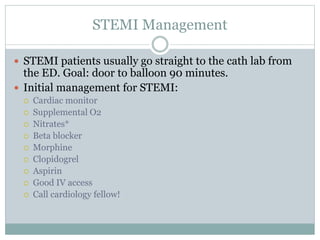
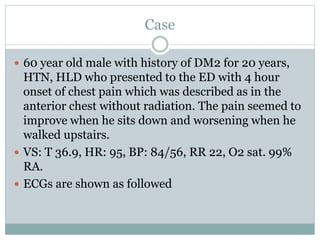
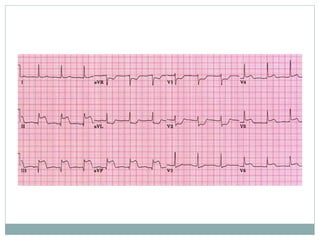
This document discusses acute coronary syndrome (ACS), including unstable angina (UA), non-ST elevation myocardial infarction (NSTEMI), and ST elevation myocardial infarction (STEMI). It defines ACS and describes how the conditions are classified based on ECG and cardiac enzyme levels. It also discusses risk stratification in NSTEMI and typical management approaches for NSTEMI, UA, and STEMI. The document concludes with a case study describing a patient presenting with chest pain.