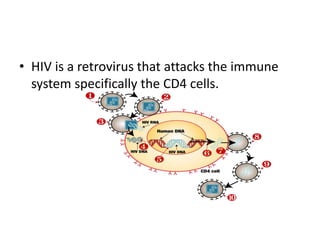
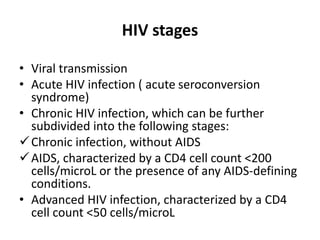
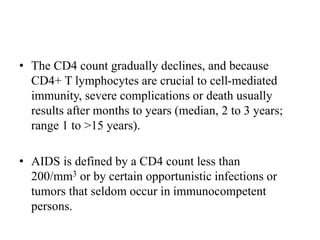
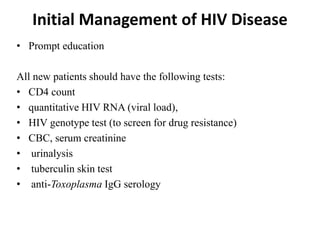
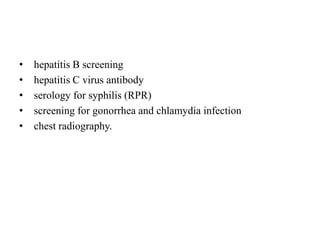
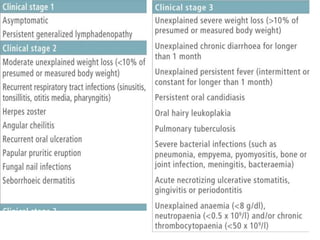
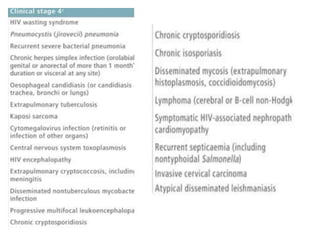
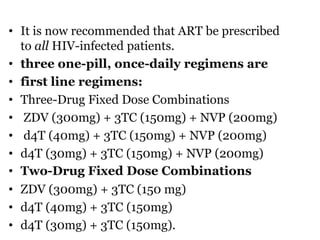
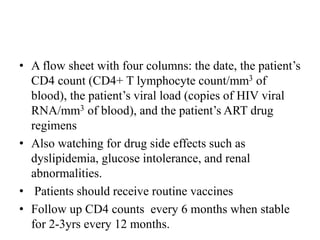
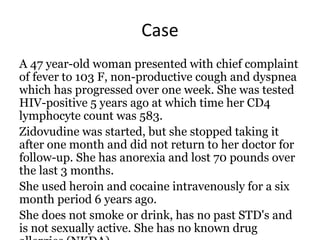
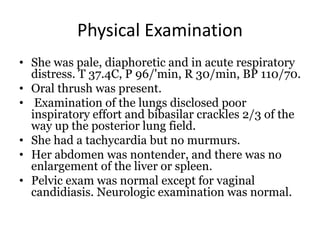
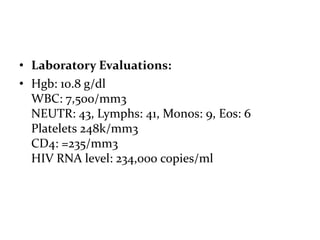
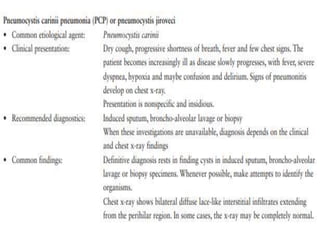
A 47-year-old woman presented with fever, cough, and difficulty breathing for one week. She was diagnosed with HIV 5 years ago but stopped treatment after one month. She now has oral thrush, tachycardia, and crackles in her lungs. Her CD4 count is low at 235 and HIV viral load is high. She is diagnosed with Pneumocystis jiroveci pneumonia, an opportunistic infection seen in advanced HIV/AIDS due to her severely compromised immune system from lack of antiretroviral treatment.