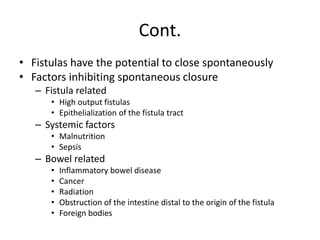
Intestinal fistulas are abnormal connections between two epithelial surfaces that can be internal or external. The majority of enterocutaneous fistulas are iatrogenic complications resulting from intestinal surgery. Clinical signs include drainage of enteric contents from surgical wounds or drains. Treatment involves stabilization, investigation to define the fistula anatomy, and rehabilitation with nutrition to allow spontaneous closure in many cases. Surgery is needed for fistulas that do not close and involves resection of the fistula tract and affected intestine. Intestinal fistulas can be challenging to treat and are associated with significant morbidity and mortality risks.