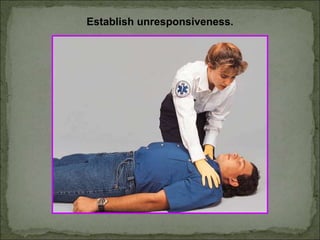
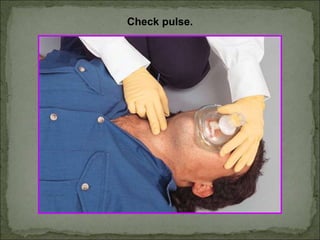
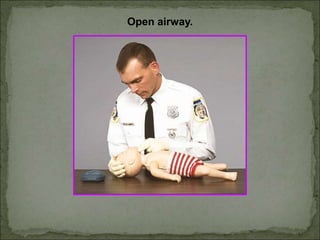
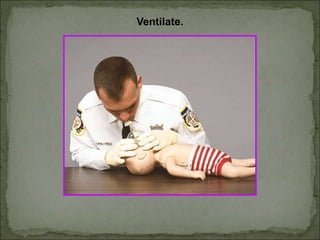
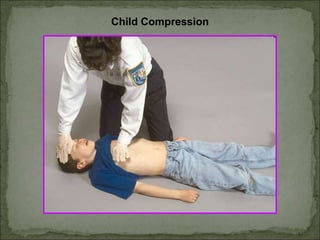
The document outlines updated recommendations for administering CPR, emphasizing effective chest compressions and a unified compression-to-ventilation ratio of 30:2 for all age groups. It stresses the importance of initiating CPR early to increase the effectiveness of defibrillation and highlights details on ventilation techniques and pulse checks. Additionally, the document compares CPR techniques for adults, children, and infants, providing guidelines for hand placement, compression depth, and rescue breathing rates.