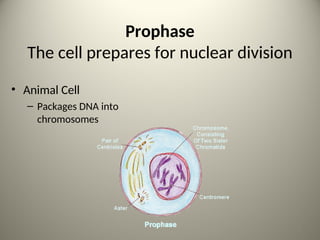
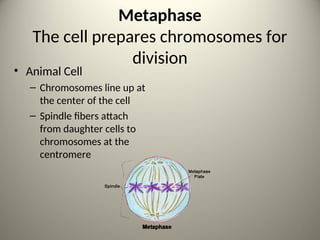
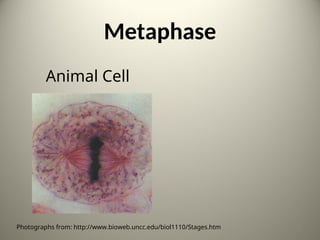
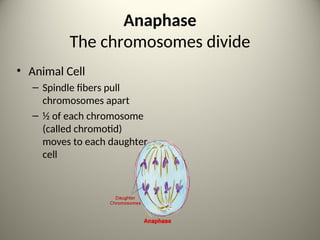
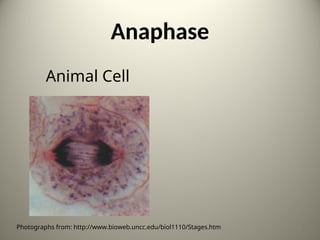
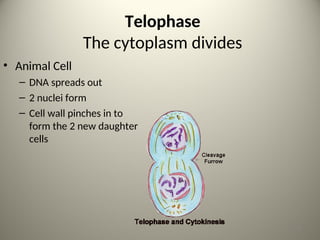
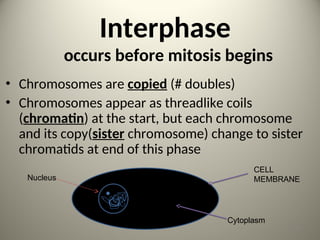
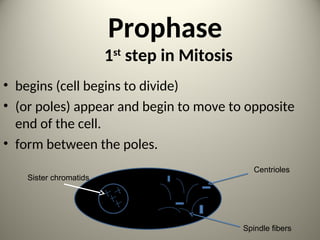
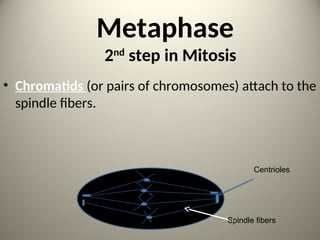
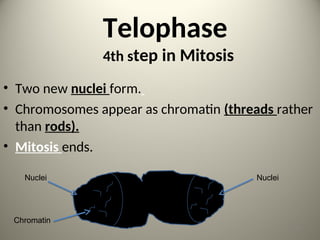
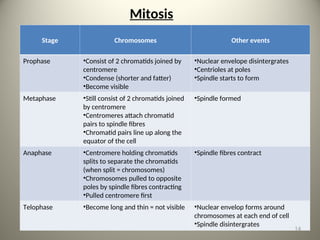
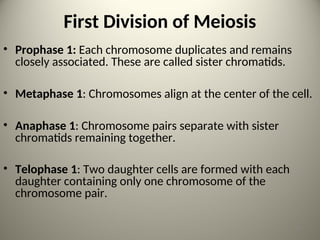
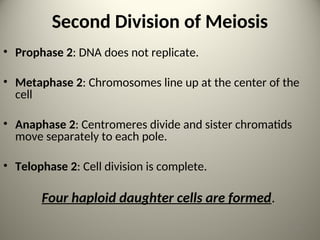
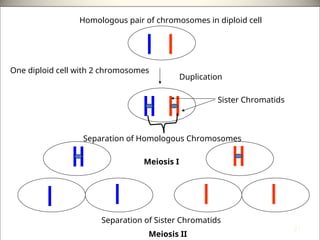
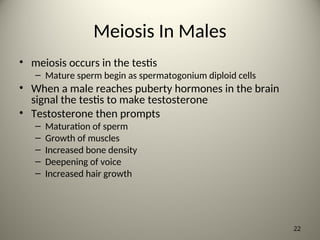
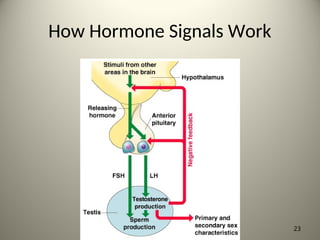
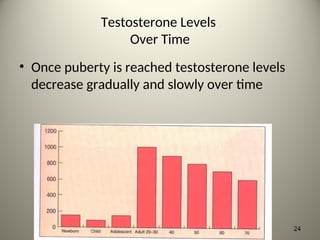
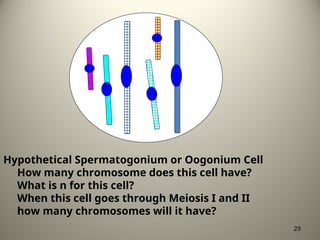
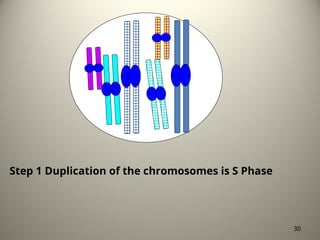
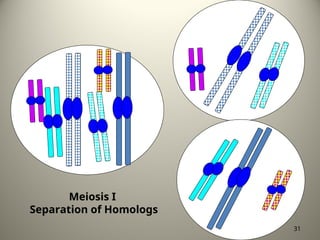
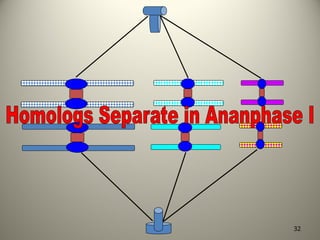
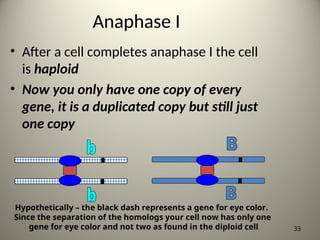
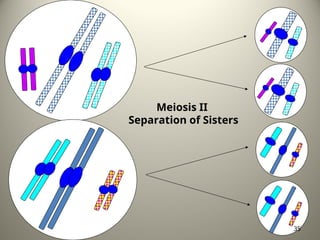
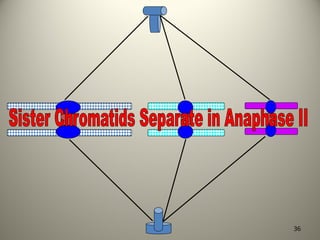
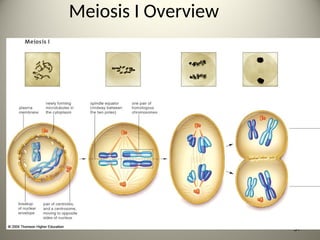
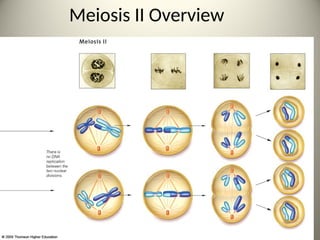
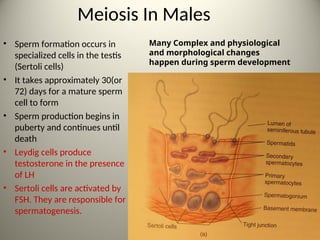
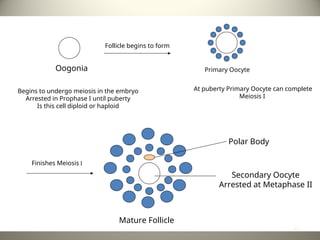
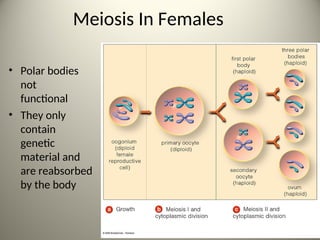
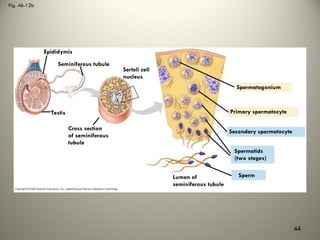
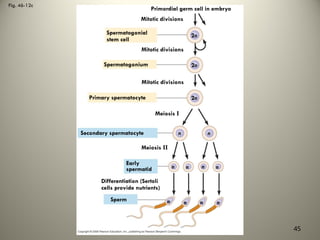
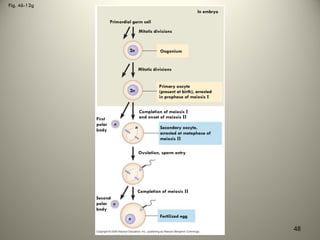
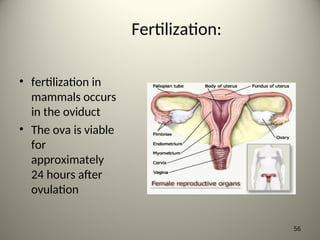
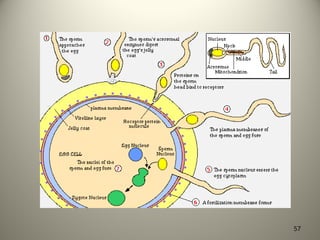
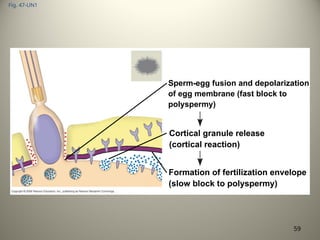
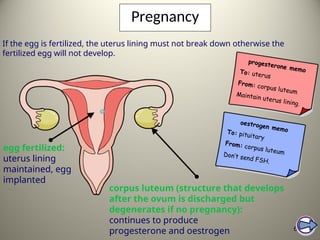
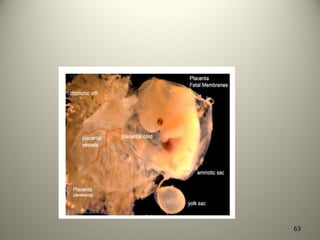
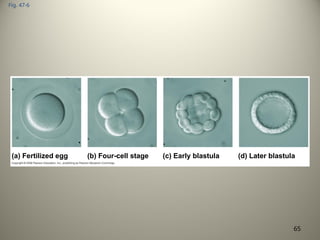
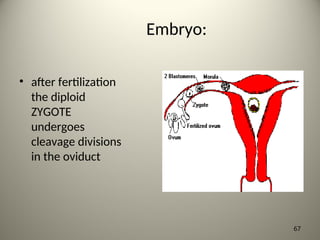
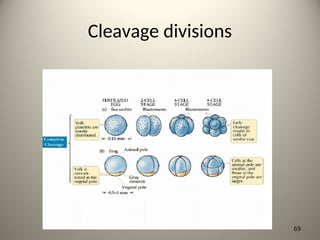
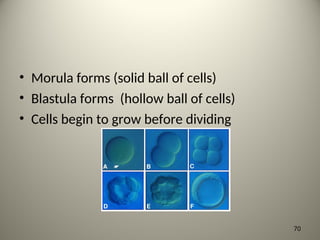
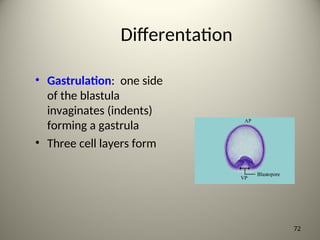
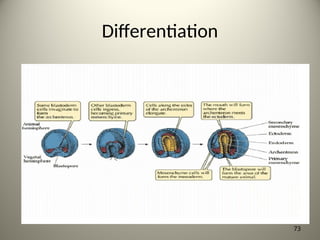
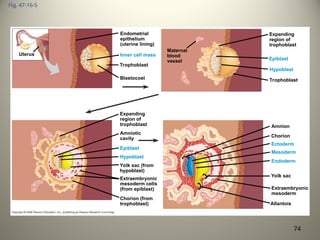
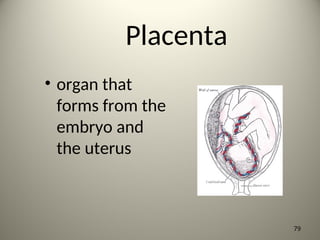
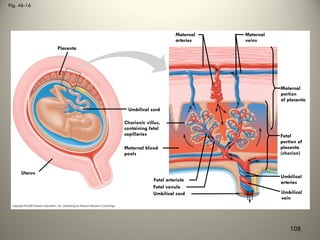
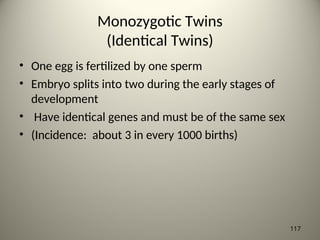
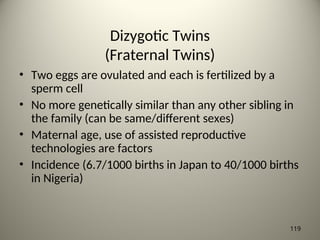
The document outlines the processes of mitosis and meiosis, focusing on the stages of each and their roles in cell division and reproduction. It details fertilization, embryonic development, and the function and structure of the placenta in mammals. Additionally, it discusses hormonal regulation in reproduction for both males and females, highlighting the differences in gametogenesis.