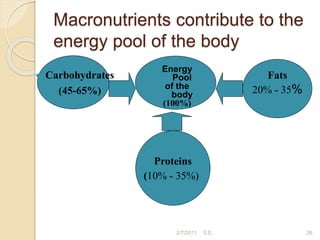
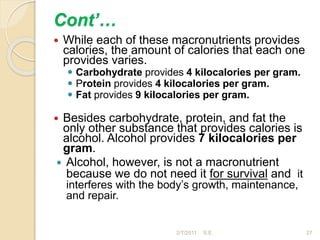
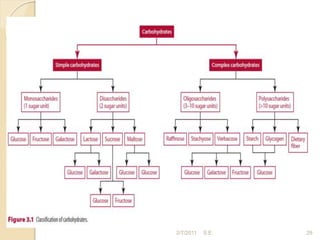
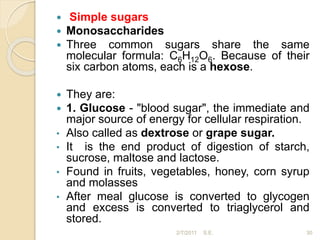
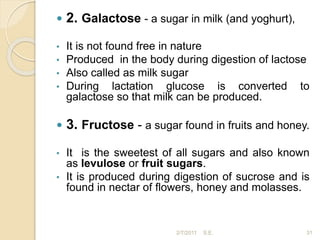
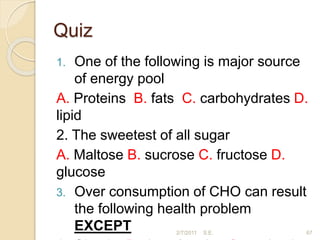
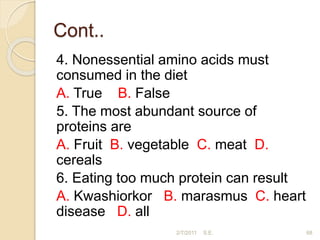
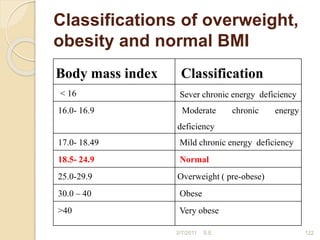
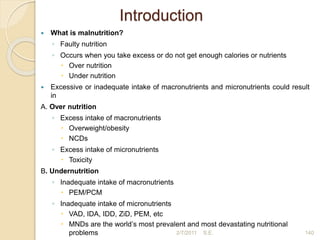
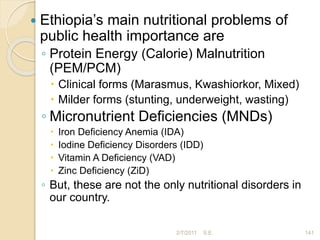
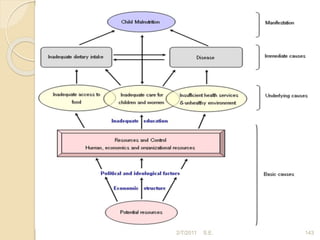
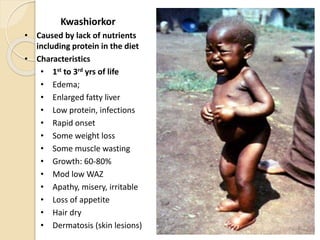
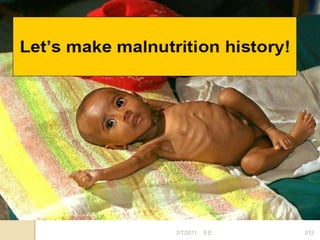
This document provides an overview of human nutrition for midwifery students. It defines key terms, classifies nutrients, and describes the six major nutrients and their functions. Carbohydrates are discussed in depth, including simple and complex forms. Malnutrition causes and consequences are also reviewed. The document aims to equip students with foundational knowledge of nutrition.