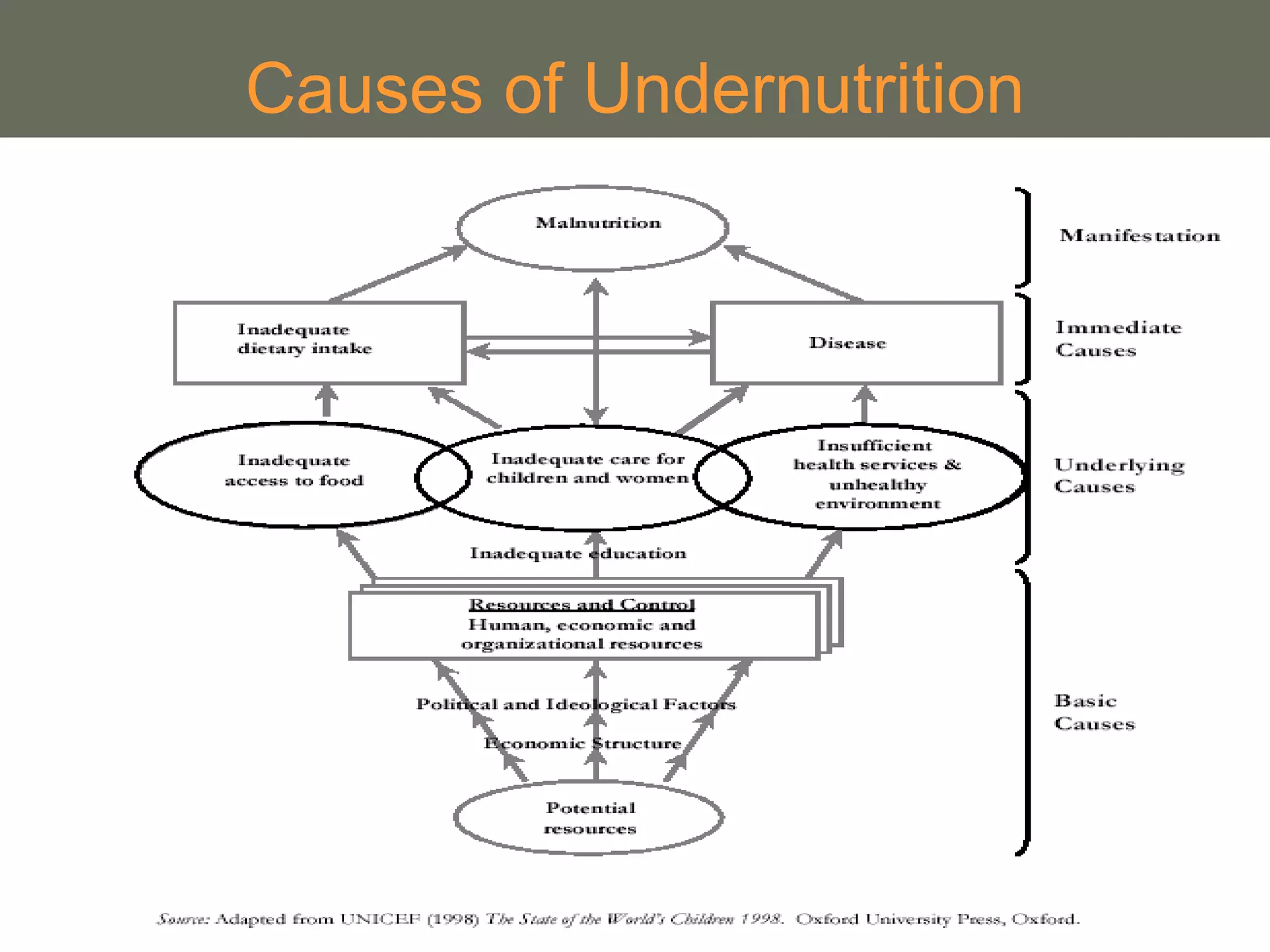
This document provides an overview of basic nutrition concepts including essential nutrients, their food sources, roles in the body, and consequences of deficiencies. It discusses national guidelines for good nutrition and combating undernutrition. Key points covered include macronutrients like carbohydrates, proteins, and fats; micronutrients like vitamins and minerals; causes and indicators of undernutrition like stunting and wasting; and strategies to prevent deficiencies such as food fortification, supplementation, and improving maternal and child nutrition.