This document provides an overview of cleft lip and palate, including:
- Incidence rates are about 1 in 1000 live births globally. Risk increases with parental age and decreases in some populations.
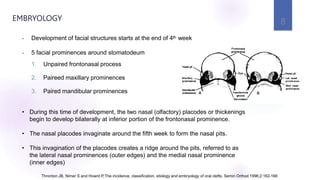
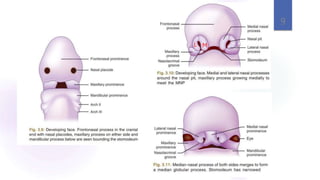
- Clefts occur due to failure of facial prominences to fuse properly during embryonic development between 4-7 weeks.
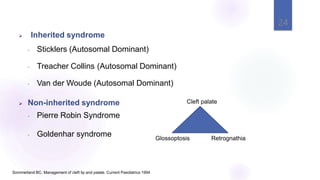
- Clefts can be non-syndromic or associated with over 350 genetic syndromes. Both genetic and environmental factors contribute to clefting.
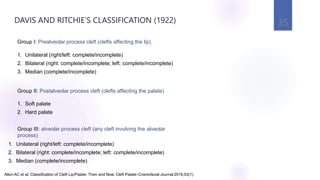
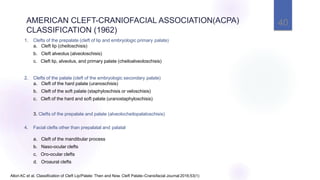
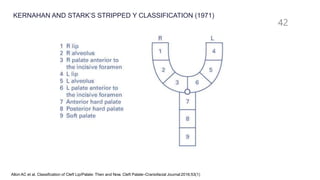
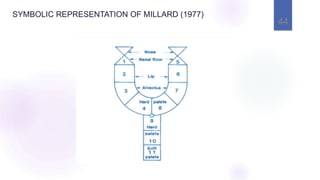
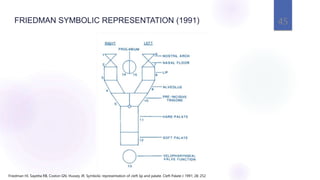
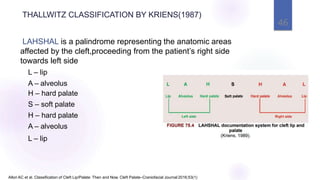
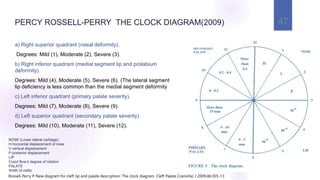
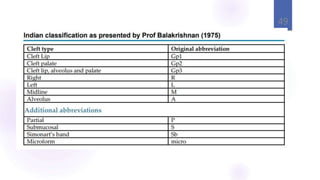
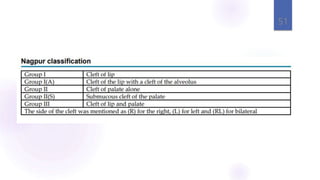
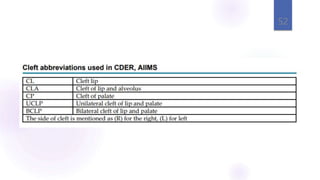
- Classification systems have evolved over time to better describe cleft types and guide multidisciplinary treatment planning. The document reviews several historic and currently used classification approaches.

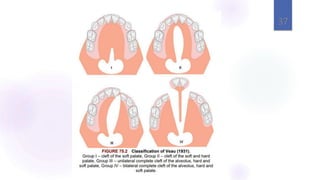
![36
A] Cleft lip
Class I : U/L notching of vermillion border, not extending into the lip.
Class II : cleft extending into the lip, but not including the floor of the nose.
Class III : extending into the floor of the nose.
Class IV : any b/l cleft of the lip, whether incomplete or complete.
B] Cleft palate
Class I : soft palate
Class II : soft/hard palate extending no further than incisive foramen.
Class III : complete unilateral cleft, extending from uvula to incisive foramen, then
deviating to one side
Class IV : two clefts extending forward from the incisive foramen into the alveolus.
Allori AC et al. Classification of Cleft Lip/Palate: Then and Now. Cleft Palate–Craniofacial Journal 2016;53(1)
VICTOR VEAU’S CLASSIFICATION (1931)](https://image.slidesharecdn.com/2cleftlipandpalate-231019051000-e53cbbe7/85/2-CLEFT-LIP-AND-PALATE-pptx-28-320.jpg)


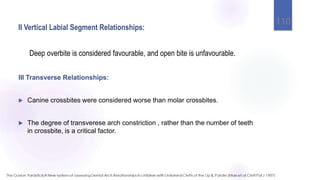
![I Anteroposterior Arch Relationships:
1. Severe Class III incisor relationships were least satisfactory[group 5]
2. class II division 1 relationship in the early permanent dentition , most
favorable for subsequent orthodontic correction.[ group 1]
3. Edge-to-edge bite is classified as group 3[fair] and negative overjet of 1–
2 mm as group 4 and negative overjet of 3–4 mm is classified as either
group 5 depending on dento alveolar inclination.
4. Pre-existing dentoalveolar compensation in the presence of a reverse
overjet was not favourable, since it limits the possible orthodontic
correction of the incisor relationship
109](https://image.slidesharecdn.com/2cleftlipandpalate-231019051000-e53cbbe7/85/2-CLEFT-LIP-AND-PALATE-pptx-76-320.jpg)