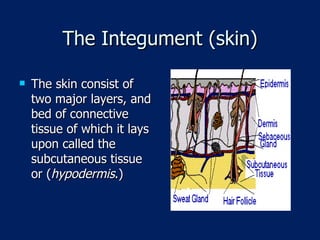
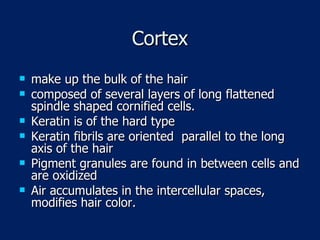
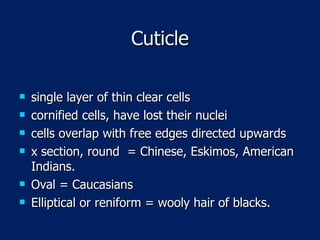
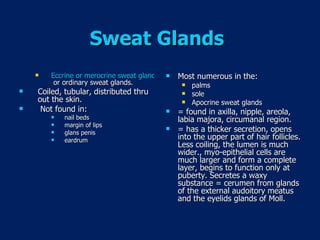
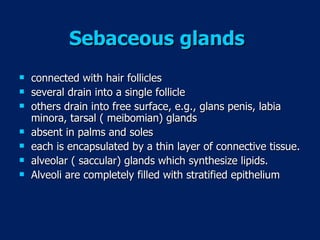
The document summarizes the structure and function of the integumentary system. It describes the two main layers of the skin - the epidermis and dermis - as well as various cell types found in the epidermis like keratinocytes, melanocytes, and Langerhans cells. It also discusses skin appendages such as hair follicles, sebaceous glands, and sweat glands. The summary concludes by noting the integumentary system acts as a protective barrier and regulates temperature and moisture.