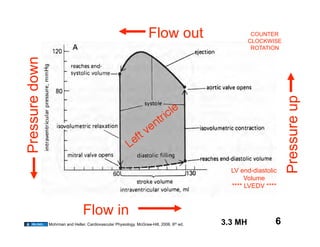
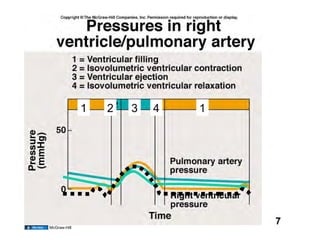
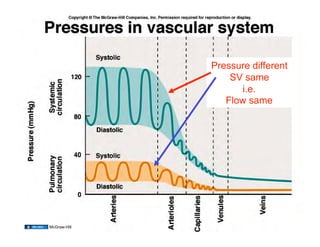
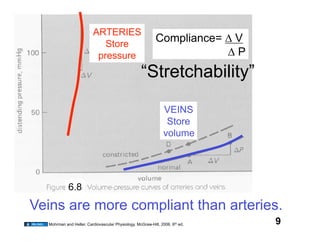
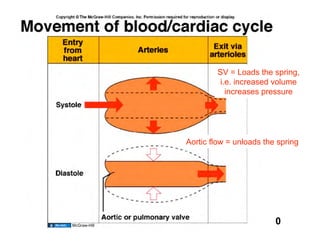
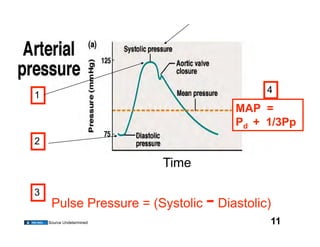
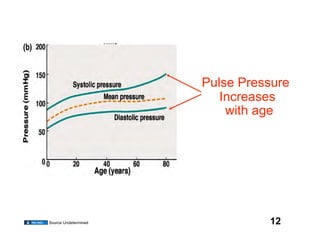
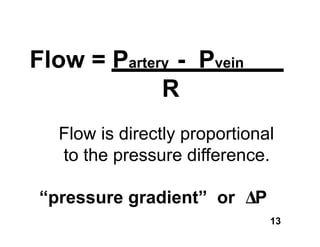
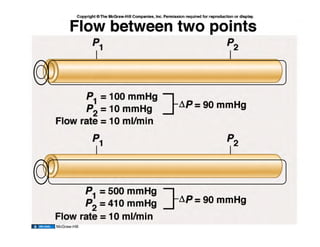
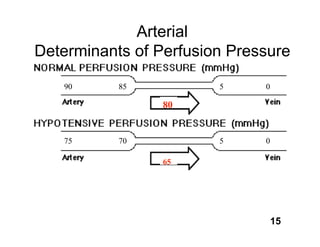
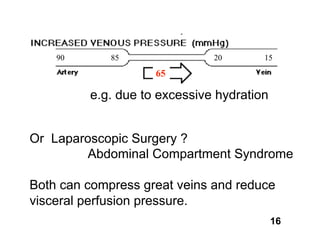
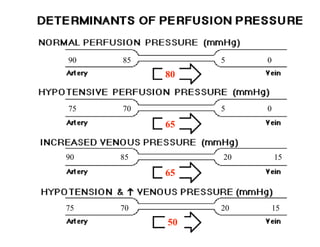
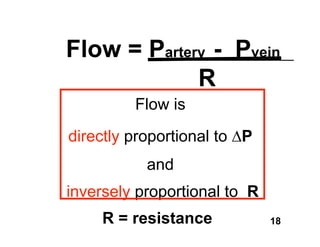
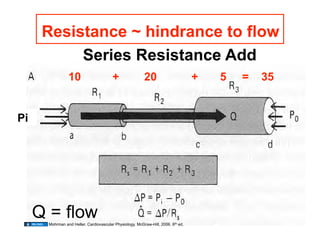
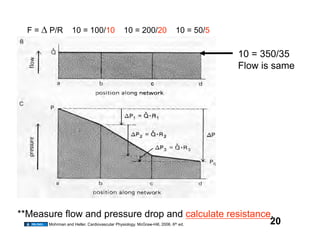
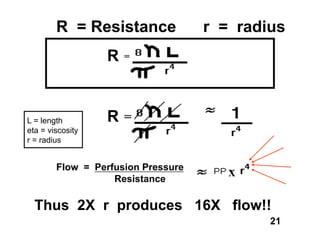
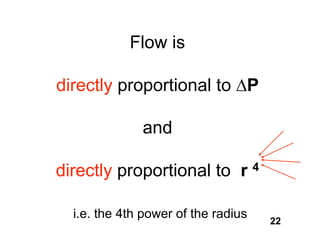
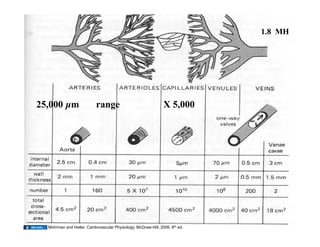
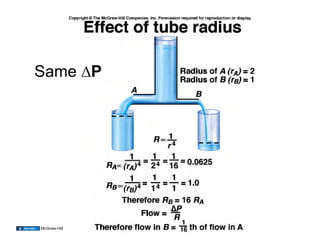
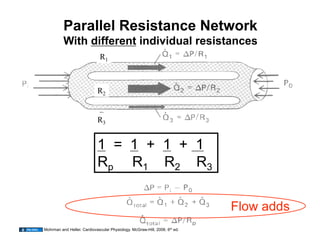
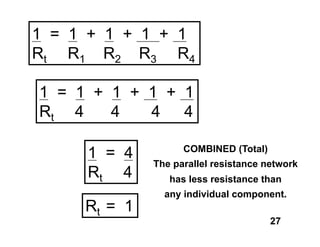
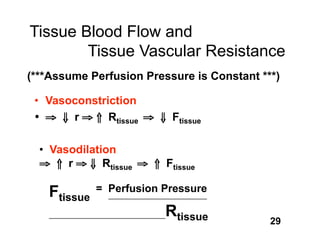
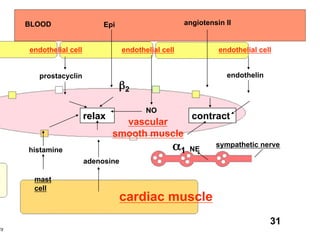
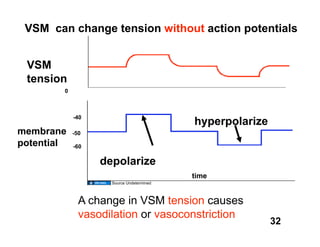
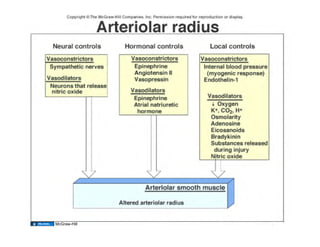
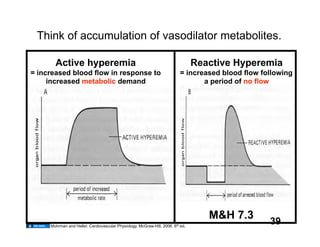
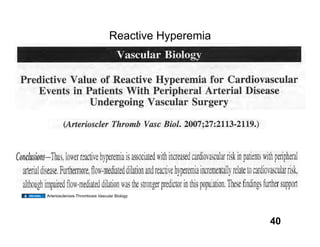
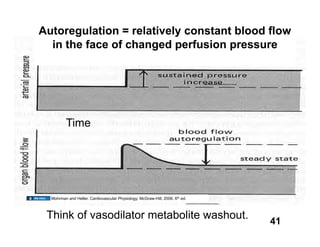
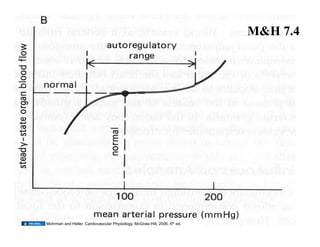
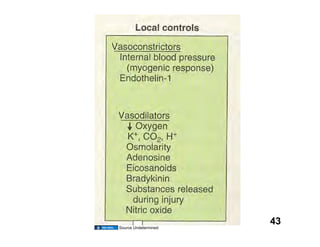
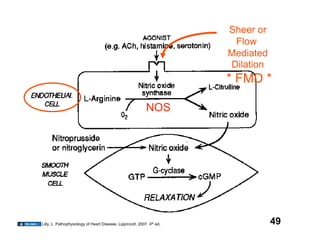
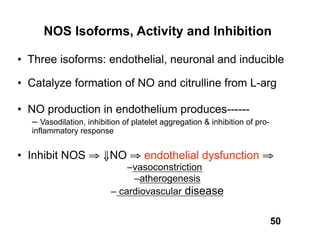
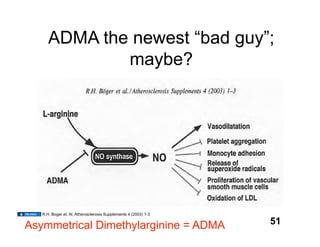
The document discusses hemodynamics, which refers to the forces generated by the heart and the motion of blood through the cardiovascular system, covering topics such as pressure, blood flow, resistance, and vascular responses to various stimuli. It emphasizes that any medical information presented is for educational purposes only and should not be used for self-diagnosis or treatment without professional advice. Additionally, it details copyright usage rights and protections related to the material, allowing for sharing and adaptation under specific conditions.