The document discusses shock, including:
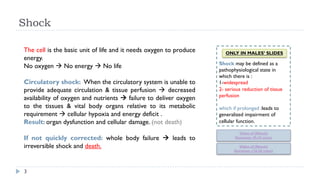
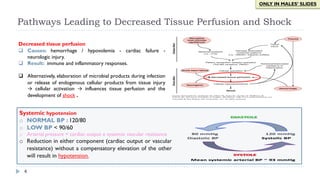
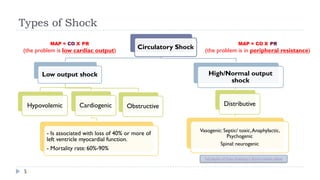
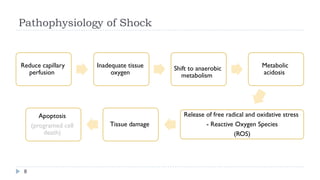
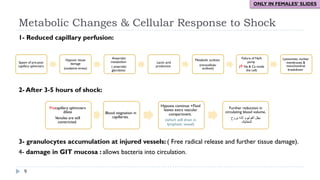
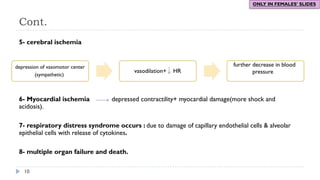
1. Circulatory shock occurs when the circulatory system is unable to provide adequate circulation and tissue perfusion, leading to cellular hypoxia and energy deficit.
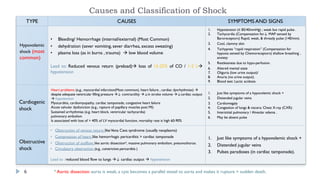
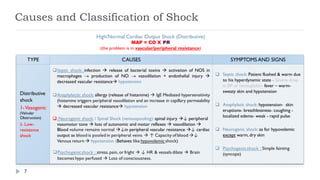
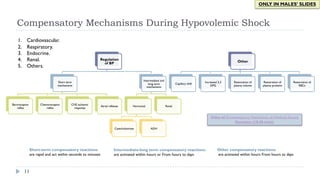
2. Shock is classified as hypovolemic, cardiogenic, obstructive, or distributive. Hypovolemic shock results from blood or fluid loss while cardiogenic shock stems from heart problems reducing cardiac output.
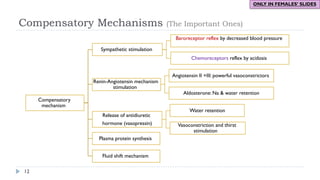
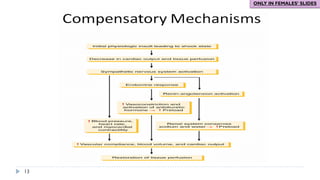
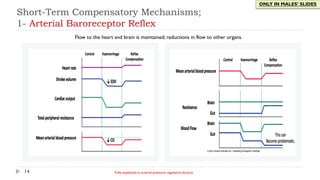
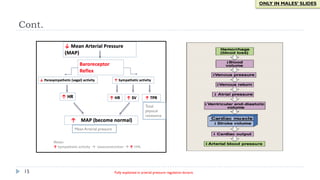
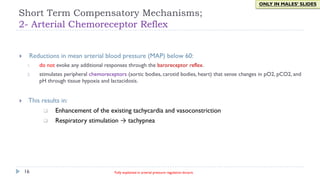
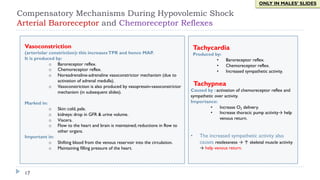
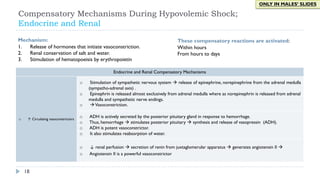
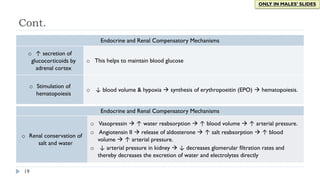
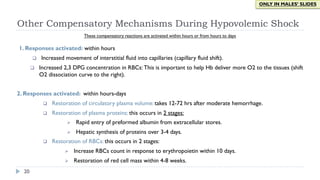
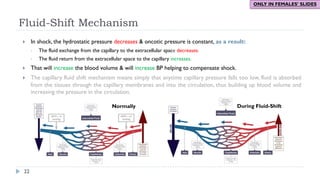
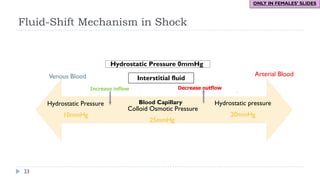
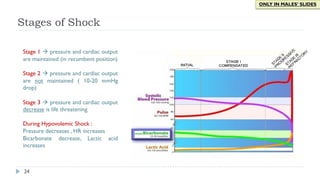
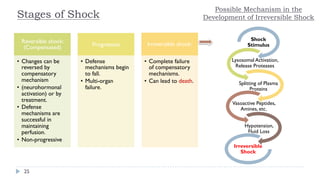
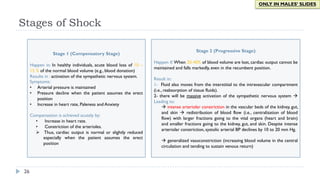
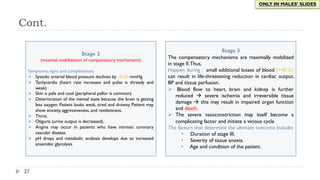
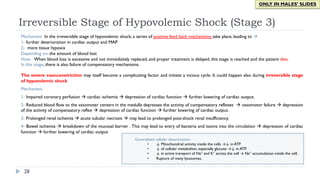
3. During the reversible phase of hemorrhagic shock, compensatory mechanisms aim to maintain perfusion through vasoconstriction, tachycardia, fluid shifts, and hormonal responses. However, irreversible shock leads to organ dysfunction and failure without rapid intervention.